Polymeric Nanoparticles for Drug Delivery: Advances, Applications, and Future Prospects
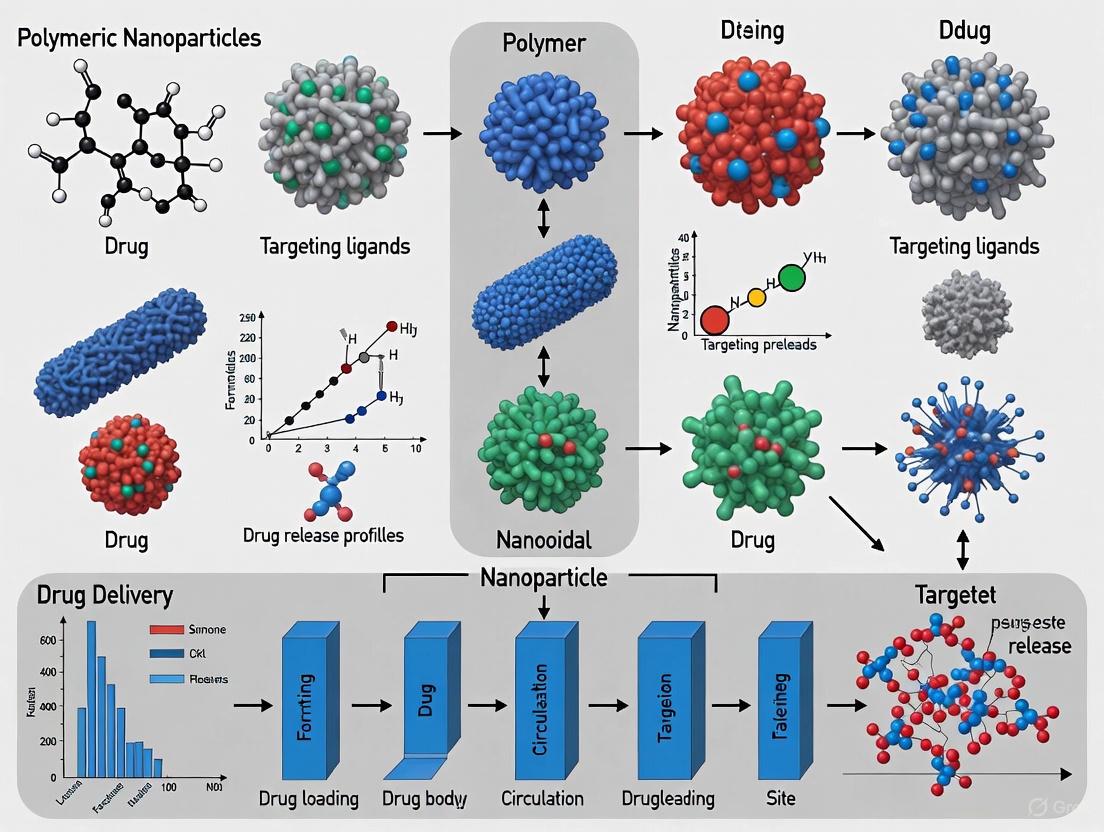
This comprehensive review explores the rapidly evolving field of polymeric nanoparticles (PNPs) as sophisticated drug delivery systems.
Polymeric Nanoparticles for Drug Delivery: Advances, Applications, and Future Prospects
Abstract
This comprehensive review explores the rapidly evolving field of polymeric nanoparticles (PNPs) as sophisticated drug delivery systems. Tailored for researchers, scientists, and drug development professionals, the article delves into the foundational principles of PNP design, including polymer selection and the biological barriers they must overcome. It provides a detailed analysis of current fabrication methodologies, characterization techniques, and their diverse therapeutic applications in areas such as cancer therapy, ocular delivery, and infectious diseases. The content further addresses critical challenges in clinical translation—including scalability, biocompatibility, and immune evasion—and offers optimization strategies. Finally, it evaluates the clinical and commercial landscape, comparing PNPs with other nanocarriers and discussing the promising integration of stimuli-responsive systems and AI-driven design for the future of precision medicine.
The Foundation of Polymeric Nanoparticles: Design Principles and Biological Interactions
Polymeric nanoparticles represent a cornerstone of modern drug delivery system research, offering unparalleled versatility in encapsulating and delivering therapeutic agents. These colloidal carrier systems, with diameters typically less than 1 μm, are primarily categorized as either nanospheres or nanocapsules based on their fundamental architectural differences [1]. Understanding this distinction is critical for researchers and drug development professionals seeking to design optimized nanocarriers for specific biomedical applications.
Nanospheres exhibit a matrix-type structure where the drug is uniformly dispersed, dissolved, or adsorbed throughout a continuous polymeric network [1]. In this configuration, the active substance is distributed within the entire volume of the solid particle, creating a monolithic system where release kinetics are governed by diffusion through the polymer matrix or polymer erosion. In contrast, nanocapsules possess a vesicular structure characterized by a core-shell morphology [1]. These systems feature an oil-based or aqueous core that encapsulates the active substance, surrounded by a protective polymeric shell that acts as a barrier membrane, controlling the release rate of the encapsulated compound. This fundamental architectural difference directly influences their drug loading capacity, release profiles, and suitability for particular therapeutic applications in drug delivery research.
Comparative Analysis: Structural and Functional Characteristics
The structural divergence between nanospheres and nanocapsules directly translates to distinct functional properties that dictate their performance in drug delivery applications. The table below summarizes the key characteristics that researchers must consider during the design phase.
Table 1: Comparative characteristics of nanospheres versus nanocapsules
| Characteristic | Nanospheres | Nanocapsules |
|---|---|---|
| Internal Structure | Matrix-based, monolithic system | Reservoir-based, vesicular system |
| Drug Location | Dispersed, dissolved, or adsorbed throughout polymer matrix | Confined within an inner cavity (oil or aqueous core) surrounded by polymeric shell [1] |
| Polymer Distribution | Uniform throughout particle | Concentrated in the shell membrane [1] |
| Typical Drug Load | Generally high for lipophilic drugs | High for lipophilic drugs (if oil core) or hydrophilic drugs (if aqueous core) |
| Release Profile | Diffusion-controlled through polymer matrix; often biphasic (initial burst followed by sustained release) | Membrane-controlled; can provide more constant, zero-order release kinetics |
| Primary Advantages | Protection of labile drugs, sustained release, high stability | High encapsulation efficiency for compatible drugs, controlled release, protection of core content |
Beyond these fundamental characteristics, the surface properties of both nanosphere and nanocapsule systems can be modified through the attachment of targeting ligands (e.g., folic acid, peptides, antibodies) to enhance site-specific accumulation [2] [3]. The polymer composition itself can be engineered to create "smart" nanoparticles that respond to specific stimuli in the tumor microenvironment (e.g., pH, redox potential, or specific enzymes), enabling precise drug release at the targeted site [3].
Preparation Methodologies: Standard Experimental Protocols
Protocol for Nanosphere Preparation via Emulsion-Solvent Evaporation
The emulsion-solvent evaporation method represents a widely utilized technique for nanosphere production, particularly suitable for encapsulating lipophilic drugs [2].
- Oil Phase Preparation: Dissolve 100-500 mg of biodegradable polymer (e.g., PLGA, PLA) and 10-50 mg of lipophilic active pharmaceutical ingredient (API) in 10-20 mL of a water-immiscible organic solvent (typically dichloromethane or ethyl acetate).
- Aqueous Phase Preparation: Prepare 50-100 mL of an aqueous surfactant solution (e.g., 0.5% - 2% w/v polyvinyl alcohol or sodium cholate) in purified water.
- Primary Emulsion Formation: Add the organic phase to the aqueous phase under high-speed homogenization (e.g., 10,000-15,000 rpm for 2-5 minutes) using a high-shear homogenizer to form an oil-in-water (O/W) emulsion.
- Solvent Evaporation: Transfer the formed emulsion to a magnetic stirrer and stir continuously at 400-600 rpm for 3-6 hours at room temperature to allow for complete evaporation of the organic solvent. This step causes the polymer to precipitate, forming solid nanospheres with the API encapsulated within the matrix.
- Purification: Centrifuge the resulting nanosphere suspension at 15,000-20,000 x g for 30-60 minutes. Discard the supernatant and re-suspend the pellet in purified water or an isotonic buffer (e.g., phosphate-buffered saline, PBS). Repeat this washing step 2-3 times to remove residual surfactant and unencapsulated API.
- Final Product Formation: Re-suspend the purified nanosphere pellet in an appropriate medium (e.g., PBS, sucrose solution for cryoprotection) and lyophilize for long-term storage, if required.
Protocol for Nanocapsule Preparation via Nanoprecipitation
The nanoprecipitation method, also known as solvent displacement, is a common and efficient technique for preparing nanocapsules with an oil core [3].
- Organic Phase Preparation: Dissolve 50-200 mg of polymer (e.g., PCL, PLA, PEG-PLA) and 5-25 mg of a lipophilic drug in a water-miscible organic solvent (e.g., acetone, ethanol). Add 0.5-2 mL of a specific oil (e.g., Miglyol 812, caprylic/capric triglycerides, or almond oil) to this solution.
- Aqueous Phase Preparation: Prepare 100-200 mL of an aqueous solution containing a stabilizer (e.g., 0.5% w/v polysorbate 20 or 80) in purified water.
- Nanoprecipitation: Inject the organic phase into the aqueous phase under moderate magnetic stirring (300-600 rpm) using a syringe pump (flow rate of 1-5 mL/min) or by drop-wise addition. The rapid diffusion of the organic solvent into the water causes the instantaneous formation of nanocapsules with an oil core surrounded by a polymeric wall.
- Organic Solvent Removal: Place the suspension under reduced pressure (e.g., using a rotary evaporator) or continue stirring for 1-2 hours at room temperature to completely remove the organic solvent.
- Purification and Concentration: Purify the nanocapsule suspension using tangential flow filtration (TFF) with appropriate molecular weight cut-off (MWCO) membranes (typically 100-300 kDa) or by centrifugation. TFF is preferred for scalable processes and to avoid capsule disruption [4].
- Final Product Formation: Adjust the concentration of the purified nanocapsules to the desired volume and lyophilize with a suitable cryoprotectant (e.g., trehalose, mannitol) for storage.
Characterization Techniques: Essential Analytical Protocols
Rigorous characterization is imperative to ensure the quality, reproducibility, and efficacy of polymeric nanoparticles. The table below outlines the critical parameters and standard analytical methods employed.
Table 2: Essential characterization techniques for polymeric nanoparticles
| Parameter | Analytical Technique | Protocol Summary & Significance | ||||
|---|---|---|---|---|---|---|
| Particle Size & Distribution (PDI) | Dynamic Light Scattering (DLS) | Dilute nanoparticle suspension in filtered buffer and measure at 25°C. PDI < 0.2 indicates a monodisperse population, crucial for reproducible biodistribution [2] [3]. | ||||
| Surface Charge | Zeta Potential Analysis | Measure electrophoretic mobility in a diluted suspension at neutral pH. A value > | +30 | mV or < | -30 | mV typically indicates good electrostatic stability [3]. |
| Encapsulation Efficiency (EE) | Indirect Method: UV-Vis Spectroscopy | Separate unencapsulated drug (via ultrafiltration/ultracentrifugation). Analyze the free drug in the supernatant. EE(%) = (Total Drug - Free Drug) / Total Drug × 100% [2]. High EE reduces cost and waste. | ||||
| Morphology | Electron Microscopy (TEM/SEM) | Deposit a diluted sample on a carbon-coated grid, stain (e.g., uranyl acetate for TEM), and image. Confirms core-shell (nanocapsules) vs. matrix (nanospheres) structure [1]. | ||||
| In Vitro Drug Release | Dialysis Bag / Franz Cell | Place nanoparticle suspension in a dialysis membrane (appropriate MWCO). Immerse in release medium (PBS, pH 7.4) at 37°C under sink conditions. Withdraw samples at predetermined times and analyze drug content via HPLC/UV-Vis to generate a release profile [1] [2]. |
The Scientist's Toolkit: Research Reagent Solutions
Successful formulation of polymeric nanoparticles requires a selection of critical reagents and materials. The following toolkit details essential components and their functions in the preparation process.
Table 3: Essential research reagents and materials for nanoparticle fabrication
| Reagent/Material | Function/Role | Common Examples |
|---|---|---|
| Biodegradable Polymers | Forms the structural matrix (nanospheres) or protective shell (nanocapsules); determines degradation rate and drug release kinetics. | Poly(lactic-co-glycolic acid) (PLGA), Poly(ε-caprolactone) (PCL), Chitosan, Poly(lactic acid) (PLA) [2] [3]. |
| Surfactants/Stabilizers | Prevents nanoparticle aggregation during and after formation by providing steric or electrostatic stabilization. | Polyvinyl Alcohol (PVA), Polysorbates (Tween), Lipoids (e.g., Lipoid S PC-3), Phospholipids [2] [5]. |
| Oils (for Nanocapsules) | Forms the internal core of nanocapsules, serving as a reservoir for dissolving and encapsulating lipophilic drugs. | Miglyol 812, Caprylic/Capric Triglycerides, Almond Oil, Ethyl Oleate [1]. |
| Organic Solvents | Dissolves polymers and lipophilic compounds for the formulation process. Must be removed to final product. | Dichloromethane (DCM), Ethyl Acetate, Acetone, Ethanol [5]. |
| Targeting Ligands | Surface-functionalization molecules that enhance specific accumulation at the target site (e.g., tumor). | Folic Acid, Peptides, Antibodies, PEG (stealth coating) [2] [3]. |
Advanced Manufacturing: Scaling Up Production
Transitioning from small-scale laboratory synthesis to industrial production presents significant challenges, including maintaining batch-to-batch reproducibility, homogeneity, and control over nanoparticle properties [5]. Conventional small-scale methods are often time-intensive and difficult to scale. A promising advancement is the use of microfluidic mixing devices for the continuous production of layer-by-layer nanoparticles [4]. This approach allows polymers and other layers to be sequentially added as particles flow through a microchannel, eliminating the need for purification after each step and integrating Good Manufacturing Practice (GMP)-compliant processes. This method has demonstrated the capability to produce 15 mg of nanoparticles (approximately 50 doses) in just a few minutes, a significant improvement over traditional batch processes, thus facilitating the path to clinical trials [4].
Polymeric nanoparticles (PNPs) represent a groundbreaking advancement in targeted drug delivery systems, offering significant benefits over conventional systems, including versatility, biocompatibility, and the ability to encapsulate diverse therapeutic agents for controlled release [6]. The selection of polymer building blocks—natural, synthetic, or a hybrid of both—is fundamental to the performance of these nanocarriers. These polymers determine the nanoparticles' critical physicochemical properties, such as size, shape, surface charge, and drug-loading capacity, which in turn influence their behavior in biological environments, targeting capabilities, and overall therapeutic efficacy [7] [6]. Framed within the context of a broader thesis on polymeric nanoparticles for drug delivery, these application notes and protocols provide a comparative overview of core polymer materials and detailed methodologies for their use in formulating advanced drug delivery systems for researchers and drug development professionals.
Comparative Analysis: Natural vs. Synthetic Polymers
The choice between natural and synthetic polymers is pivotal and depends on the specific requirements of the drug delivery application. The table below summarizes their key characteristics and applications.
Table 1: Comparative Analysis of Natural and Synthetic Polymers for Drug Delivery
| Feature | Natural Polymers | Synthetic Polymers |
|---|---|---|
| Origin | Extracted from microorganisms, algae, plants, or animals (e.g., crustaceans) [7]. | Artificially produced in laboratories from petroleum-derived monomers [7]. |
| Common Examples | Alginate, hyaluronic acid, chitosan, collagen, gelatin, starch [7]. | Poly(lactic acid) (PLA), Poly(lactic-co-glycolic acid) (PLGA), Poly(vinyl alcohol) (PVA), Polyethylene glycol (PEG) [7] [6]. |
| Backbone Composition | Carbon, oxygen, nitrogen [7]. | Predominantly carbon-carbon bonds [7]. |
| Biocompatibility & Toxicity | Generally high biocompatibility; similar to ECM components, avoiding chronic immunological reactions [7]. | Variable; many are biocompatible and biodegradable, but some can elicit toxicity or immune responses [7] [8]. |
| Biodegradability | Usually biodegradable and metabolized in the biological environment [7]. | Some are biodegradable (e.g., PLA, PLGA); others are not [7]. |
| Key Advantages | Biocompatible, biodegradable, low carbon footprint, often biologically active (e.g., inherent antibacterial properties of chitosan) [7]. | Properties can be precisely engineered (e.g., molecular weight, degradation rate); high batch-to-batch consistency; versatile chemistry for functionalization [7] [8]. |
| Key Limitations | Batch-to-batch variability; strong intra/intermolecular bonds can limit processability; potential immunogenicity [7] [8]. | Risk of toxicity or biopersistence from non-degradable polymers or degradation by-products; complex manufacturing scaling [8]. |
| Primary Drug Delivery Applications | Drug delivery carriers, tissue engineering scaffolds, wound healing, hydrogel preparation [7]. | Controlled drug release systems, nano-carriers, stimuli-responsive "smart" systems, gene delivery, bio-inks for 3D-printing [7] [6]. |
Application Notes and Experimental Protocols
Protocol: Formulation of Stimuli-Responsive Hybrid Nanoparticles
This protocol details the synthesis of near-infrared (NIR) light-responsive hybrid particles for controlled drug and growth factor release, adapted from recent research [7].
3.1.1. Principle Hybrid particles composed of natural proteins (gelatin, agarose) and black phosphorus quantum dots (BPQDs) are engineered to release encapsulated cargo (e.g., antimicrobial peptides, growth factors) upon exposure to NIR light. The BPQDs absorb NIR light, generating heat that induces a reversible phase transition in the gelatin matrix, thereby liberating the therapeutic payload [7].
3.1.2. Materials
- Gelatin (Natural polymer): Thermoresponsive matrix material.
- Agarose (Natural polymer): Provides structural integrity to the particle.
- Black Phosphorus Quantum Dots (BPQDs): NIR-responsive photothermal agent.
- Therapeutic Cargo: e.g., Vascular Endothelial Growth Factor (VEGF), antimicrobial peptides.
- Phosphate Buffered Saline (PBS): For buffer preparation.
- Source of NIR Light: e.g., NIR laser (808 nm).
3.1.3. Procedure
- BPQD Synthesis: Prepare BPQDs via liquid exfoliation of bulk black phosphorus in an organic solvent under an inert atmosphere.
- Polymer Solution Preparation: Dissolve gelatin and agarose in warm PBS (at approximately 40-50°C) under gentle stirring to form a homogeneous solution.
- Cargo Loading: Add the therapeutic cargo (e.g., VEGF) and the synthesized BPQDs to the polymer solution. Mix thoroughly to ensure even distribution.
- Particle Formation: Emulsify the mixture in a cold oil phase under high-speed homogenization to form water-in-oil (W/O) emulsion droplets. Cool the emulsion on an ice bath to solidify the particles.
- Washing and Collection: Centrifuge the particles, discard the oil phase, and wash the collected particles multiple times with PBS to remove residual oil and unencapsulated materials.
- Storage: Store the final hybrid particles in PBS at 4°C until use.
3.1.4. Release Kinetics Assessment
- Suspend a known quantity of drug-loaded particles in a release medium (e.g., PBS) in a vial.
- Place the vial in a temperature-controlled shaker.
- At predetermined time intervals, expose the sample to NIR light (e.g., 808 nm laser at a specific power density) for a set duration.
- Following irradiation, centrifuge the samples and collect the supernatant.
- Analyze the supernatant using an appropriate method (e.g., HPLC, ELISA) to quantify the amount of drug released.
- Plot the cumulative drug release versus time to characterize the release profile.
Protocol: Layer-by-Layer (LbL) Assembly for Colon-Targeted Drug Delivery
This protocol describes the fabrication of a multilayered nanocapsule system for targeted oral delivery of biologics like insulin, preventing premature release in the upper gastrointestinal tract (GIT) [9].
3.2.1. Principle LbL assembly involves the alternating deposition of polyelectrolytes with opposing charges onto a core template (e.g., a protein). The number, composition, and compactness of these layers dictate the release kinetics and targeting specificity of the encapsulated biologic [9].
3.2.2. Materials
- Core Biologic: e.g., Insulin (IN).
- Polyelectrolytes: Carboxymethyl starch (CMS, anionic) and Spermine-modified starch (SS, cationic).
- pH-adjusted Buffers: For dissolving and washing layers at optimal pH.
3.2.3. Procedure
- Core Preparation: Dissolve insulin in a buffer at a pH where it carries a net positive charge.
- First Layer Deposition: Under constant stirring, add a solution of anionic CMS to the insulin solution. The CMS will adsorb onto the insulin surface, reversing the surface charge.
- Washing: Centrifuge the obtained IN/CMS particles and re-disperse in fresh buffer to remove non-adsorbed polyelectrolyte.
- Second Layer Deposition: Add a solution of cationic SS to the IN/CMS dispersion. The SS will adsorb onto the anionic surface, forming an IN/CMS/SS nanocapsule.
- Iterative Layering: Repeat the washing and deposition steps to add subsequent layers (e.g., another CMS layer to form IN/CMS/SS/CMS) until the desired number of layers is achieved.
- Critical Parameter Optimization: Systematically vary the ratio of CMS:SS (e.g., 1:2, 1:4, 1:8) during the assembly process. This directly impacts shell compactness, particle size, zeta potential, and ultimately, the release profile [9].
3.2.4. In Vitro Release Testing in Simulated GIT
- Simulated Gastric Fluid (SGF): Incubate the LbL nanocapsules in SGF (pH ~1.2) for a set period (e.g., 2 hours) to simulate stomach transit.
- Simulated Intestinal Fluid (SIF): Transfer the capsules to SIF (pH ~6.8) for a further period to simulate small intestine transit.
- Simulated Colonic Fluid (SCF): Finally, transfer to SCF (often at a higher pH or with specific enzymes) to simulate the colon.
- At each stage, sample the release medium, and quantify the amount of insulin released. A well-designed system will show minimal release in SGF and SIF, with the majority of release triggered in SCF.
Table 2: Impact of CMS:SS Ratio on LbL Nanocapsule Properties and Release Profile [9]
| CMS:SS Ratio | Particle Size (nm) | Zeta Potential (mV) | Premature Insulin Release in Upper GIT |
|---|---|---|---|
| 1:2 | ~26.6 | +3.7 | High (~60%) |
| 1:4 | ~16.0 | +8.9 | Moderate (~26%) |
| 1:8 | ~14.5 | +11.7 | Low (~12%) |
Visualization of Workflows and Relationships
Polymer Selection and Nanoparticle Fabrication
Mechanism of Stimuli-Responsive Drug Release
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Polymeric Nanoparticle Research
| Reagent/Material | Function/Application | Examples |
|---|---|---|
| Chitosan | Natural polymer; mucoadhesive, inherent antibacterial properties; used in wound healing patches and microneedle arrays [7]. | CSMNA patches for wound healing [7]. |
| Poly(lactic-co-glycolic acid) (PLGA) | Synthetic, biodegradable polymer; provides controlled release profiles; widely used in microspheres and implants [6] [8]. | Lornoxicam-loaded microspheres for intra-articular administration [6]. |
| Polyethylene Glycol (PEG) | Synthetic polymer; used for "PEGylation" to impart stealth properties, reduce opsonization, and extend circulation time [6] [8]. | Surface coating on liposomes (Doxil) and polymeric nanoparticles [8]. |
| Carboxymethyl Starch (CMS) | Modified natural polymer (anionic); used as a polyelectrolyte in LbL assembly for oral colon-targeted delivery [9]. | LbL nanocapsules for insulin delivery [9]. |
| Black Phosphorus Quantum Dots (BPQDs) | Photothermal agent; enables stimuli-responsive drug release when incorporated into natural polymer matrices like gelatin [7]. | NIR-light responsive hybrid particles for wound healing [7]. |
| Targeting Ligands | Molecules (antibodies, peptides, folates) conjugated to nanoparticle surface to enable active targeting to specific cells (e.g., tumor cells) [6]. | EGF fusion protein for targeting EGFR+ tumors; folic acid for folate-receptor positive cancers [9] [6]. |
The efficacy of a therapeutic agent is fundamentally governed by its ability to reach its site of action in sufficient concentration. Biological barriers—systemic, microenvironmental, and cellular—represent a formidable challenge in drug delivery, often preventing promising candidates from achieving their full therapeutic potential [10]. Polymeric nanoparticles (PNPs) have emerged as a groundbreaking platform to navigate this complex landscape. Their versatility, biocompatibility, and capacity for engineered control allow for enhanced drug bioavailability, specific targeting, and minimized off-target effects [11] [12]. This document outlines the key biological hurdles and provides detailed application notes and protocols for using PNPs to overcome them, framed within contemporary drug delivery research.
Biological barriers operate at multiple levels, from the entire organism down to subcellular compartments. The table below categorizes these hurdles and summarizes how PNP-based strategies can address them.
Table 1: Classification of Biological Barriers and PNP Countermeasures
| Barrier Category | Specific Example | Impact on Drug Delivery | PNP-Based Strategy |
|---|---|---|---|
| Systemic Barriers | Rapid clearance by immune system (MPS), Enzymatic degradation in blood [13] [10] | Short circulation half-life, reduced bioavailability | Surface PEGylation to impart "stealth" properties, use of biodegradable polymers [12] [14] |
| Microenvironmental Barriers | Blood-Brain Barrier (BBB), Tumor Microenvironment (acidic pH, high ROS, enzymatic activity) [10] [15] | Prevents drug access to target tissue, reduces efficacy | Stimuli-responsive (pH, redox, enzyme) polymers; surface functionalization with targeting ligands (e.g., peptides, antibodies) [12] [16] |
| Cellular Barriers | Cell membrane, Endolysosomal entrapment, Nuclear envelope [10] | Limits intracellular drug delivery, leads to drug degradation | Cell-penetrating peptides (CPPs), endosomolytic agents, nuclear localization signals [12] |
The Scientist's Toolkit: Essential Reagents and Materials
The development and evaluation of advanced PNPs require a suite of specialized reagents and materials.
Table 2: Key Research Reagent Solutions for PNP Formulation and Testing
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Biodegradable Polymers | Form the nanoparticle matrix; control drug release kinetics. | PLGA, Chitosan, Poly(lactic acid) (PLA), Poly(ε-caprolactone) (PCL) [11] [12] [17] |
| Stimuli-Responsive Polymers | Enable triggered drug release in response to specific pathological cues. | pH-sensitive polymers (e.g., poly(β-amino esters)), redox-sensitive polymers (e.g., with disulfide linkages) [12] [16] |
| Targeting Ligands | Direct PNPs to specific cells or tissues (active targeting). | Antibodies or fragments, peptides (e.g., RGD), folates, aptamers [12] [14] |
| Stabilizers & Surfactants | Control nanoparticle size and stability during fabrication. | Polyvinyl Alcohol (PVA), Poloxamers (Pluronic F127, F68) [11] |
| In Vitro Barrier Models | Preclinical evaluation of PNP penetration and transport. | Transwell assays, Organ-on-a-chip models (e.g., liver-on-a-chip, BBB-on-a-chip) [18] [14] [15] |
Experimental Protocols
Protocol: Formulation of PEGylated PLGA Nanoparticles via Nanoemulsion
This protocol describes the preparation of core PNPs with a "stealth" coating to evade the immune system [11] [12].
Application Note: This method is ideal for encapsulating hydrophobic drugs and establishing a long-circulating nanocarrier platform for systemic administration.
Materials:
- Polymer: PLGA (50:50, acid-terminated)
- Surfactant: Polyvinyl Alcohol (PVA, 1-5% w/v aqueous solution)
- PEGylation Agent: PLGA-PEG diblock copolymer
- Organic Solvent: Ethyl acetate
- Drug: Model compound (e.g., Docetaxel)
- Equipment: Probe sonicator, magnetic stirrer, centrifugation system
Procedure:
- Organic Phase Preparation: Dissolve 100 mg of PLGA and 10 mg of PLGA-PEG in 5 mL of ethyl acetate. Add the drug (e.g., 10 mg Docetaxel) and vortex until fully dissolved.
- Aqueous Phase Preparation: Place 20 mL of 2% w/v PVA solution in a 50 mL glass beaker.
- Nanoemulsion Formation: While vigorously stirring the aqueous phase, add the organic phase dropwise. Subsequently, probe sonicate the mixture on ice (100 W, 60% amplitude) for 2 minutes to form a stable oil-in-water nanoemulsion.
- Solvent Evaporation: Stir the emulsion overnight at room temperature to allow for complete evaporation of the organic solvent and nanoparticle hardening.
- Purification: Centrifuge the nanoparticle suspension at 15,000 rpm for 30 minutes at 4°C. Wash the pellet with ultrapure water to remove excess PVA and unencapsulated drug. Repeat centrifugation twice.
- Characterization: Re-disperse the final nanoparticle pellet in PBS or water. Characterize for size, polydispersity index (PDI), and zeta potential using dynamic light scattering (DLS). Determine drug loading and encapsulation efficiency via HPLC.
Protocol: Fabrication of pH-Responsive PNPs for Tumor Targeting
This protocol outlines the synthesis of PNPs that release their payload in response to the acidic tumor microenvironment [12] [16].
Application Note: These nanoparticles are designed to exploit the enhanced permeability and retention (EPR) effect and provide site-specific drug release, minimizing systemic toxicity.
Materials:
- Polymer: pH-sensitive polymer (e.g., Poly(β-amino ester))
- Crosslinker: Cystamine (for redox sensitivity)
- Drug: Doxorubicin hydrochloride
- Equipment: Dialysis tubing, magnetic stirrer, pH meter
Procedure:
- Polymer Dissolution: Dissolve 50 mg of the pH-sensitive polymer in 4 mL of dimethyl sulfoxide (DMSO).
- Drug Loading: Add a solution of 5 mg Doxorubicin in 1 mL of DMSO to the polymer solution. Stir gently for 1 hour.
- Nanoparticle Self-Assembly: Transfer the polymer-drug solution into a dialysis tube (MWCO: 3.5-7 kDa). Dialyze against a 100x volume of phosphate-buffered saline (PBS, pH 7.4) for 24 hours, changing the buffer every 6-8 hours. During dialysis, the nanoparticles will self-assemble as the solvent is exchanged.
- Crosslinking (Optional): To add dual pH/redox sensitivity, add cystamine dihydrochloride and a carbodiimide crosslinker to the nanoparticle suspension and stir for 4 hours. Purify via dialysis.
- Characterization and Release Testing: Characterize the nanoparticles as in Protocol 4.1. Perform in vitro drug release studies using dialysis in PBS at pH 7.4 and pH 5.5 (simulating the tumor microenvironment) to confirm pH-responsive release.
Visualization of PNP Trafficking and Overcoming Cellular Barriers
The following diagram illustrates the sequential journey of a targeted, stimuli-responsive PNP from systemic circulation to intracellular action.
Diagram 1: PNP Journey from Circulation to Action
Workflow for Evaluating PNP Performance Against Biological Barriers
A standardized workflow is crucial for systematically assessing how well novel PNPs overcome key hurdles.
Diagram 2: PNP Performance Evaluation Workflow
Within the field of polymeric nanoparticle (PNP) drug delivery systems, the protein corona (PC) represents a critical, yet often overlooked, interface that dictates the ultimate biological fate of administered nanocarriers. Upon introduction to any biological fluid (e.g., blood, amniotic fluid), nanoparticles are immediately coated by a dynamic layer of proteins, forming the PC. This corona confers a new "biological identity" that fundamentally redefines how the nanoparticle interacts with cells and tissues, overriding its initial synthetic design [19] [20] [21]. For researchers and drug development professionals, a deep understanding of the PC is no longer optional but essential for rational nanocarrier design. The PC influences every aspect of in vivo performance, including cellular uptake, biodistribution, targeting efficacy, and potential toxicity [20] [22]. This Application Note details the core principles of PC formation, provides quantitative data on its composition and effects, and outlines standardized protocols for its investigation, specifically within the context of advancing PNP-based therapeutic and diagnostic applications.
Core Concepts and Quantitative Data
The Dual Nature of the Protein Corona and Key Influencing Factors
The PC is typically categorized into two layers: the hard corona, consisting of proteins with high affinity that are tightly and almost irreversibly bound to the nanoparticle surface, and the soft corona, comprising proteins that are loosely bound and engaged in dynamic, transient exchange with the surrounding environment [19] [20]. The hard corona is thermodynamically favorable and plays the predominant role in determining the nanoparticle's biological identity [19].
The composition and density of the PC are governed by a complex interplay of nanoparticle physicochemical properties and the nature of the biological environment, as shown in the diagram below.
Diagram Title: Factors Governing Protein Corona Formation
Key Factors Influencing PC Formation:
- Nanoparticle Physicochemical Properties: Size and surface chemistry are primary determinants. Smaller nanoparticles have a higher curvature that influences protein binding affinity. Surface charge (zeta potential) directs electrostatic interactions with proteins, while hydrophobicity drives adsorption through hydrophobic forces [20]. The presence of surface functional groups, such as PEG, can dramatically reduce total protein adsorption and create a "stealth" effect [19] [23].
- Biological Environment Factors: The source and concentration of proteins (e.g., plasma vs. amniotic fluid) lead to distinct coronas. Physiological conditions like pH and temperature, as well as the duration of exposure (time), further modulate the corona's composition and dynamics, a phenomenon described by the Vroman effect [20] [22].
Impact of Polymer Type and PEGylation on the Protein Corona
The core polymer and surface architecture of PNPs directly determine the PC's properties, which in turn dictate cellular association and in vivo biodistribution. The following table summarizes experimental data from a study investigating polymeric nanoparticles for intra-amniotic delivery [19] [24].
Table 1: Protein Corona Characteristics and Biological Effects of Different Polymeric Nanoparticles in Amniotic Fluid
| Nanoparticle Type | Hydrodynamic Diameter (nm) | Surface Charge (mV) | Key Proteins in Corona | In Vitro Cellular Association | Primary In Vivo Biodistribution (Fetal) |
|---|---|---|---|---|---|
| PLGA | ~140-190 [19] | -6 to -10 [19] | Not Specified | Low [24] | Not Detected [24] |
| PLGA-PEG | ~140-190 [19] | -6 to -10 [19] | High Albumin [24] | High [24] | Lung [24] |
| PLA-PEG | ~140-190 [19] | -6 to -10 [19] | Keratins [24] | Not Specified | Bowel [24] |
| PACE-PEG | ~140-190 [19] | ~+5 [19] | High Albumin [24] | High [24] | Lung [24] |
Critical Insights from the Data:
- The Role of PEGylation: Surface PEGylation creates a dense brush conformation that confers a "stealth" property, significantly enhancing colloidal stability in biological fluids like amniotic fluid. This stability is crucial for successful in vivo delivery, as non-PEGylated NPs (PLGA) failed to distribute to fetal organs [19] [24].
- Corona Composition Drives Targeting: The specific protein profile in the corona is linked to organ-specific targeting. PLGA-PEG and PACE-PEG NPs, which accumulated high levels of albumin in their corona, showed preferential distribution to the fetal lung. In contrast, PLA-PEG NPs, with a corona rich in keratins, distributed exclusively to the fetal bowel, suggesting that pre-adsorbed proteins can act as endogenous targeting ligands [24].
- Cellular Association Correlation: In vitro experiments on A549 cells demonstrated a direct correlation between the amount of albumin in the PC and the level of cellular association, highlighting how the PC directly mediates cell-NP interactions [24].
Experimental Protocols
This section provides a detailed methodology for isolating and characterizing the protein corona formed on polymeric nanoparticles, a fundamental prerequisite for understanding their biobehavior.
Protocol: Protein Corona Isolation and Characterization via Density Gradient Ultracentrifugation
This protocol is adapted from advanced methods developed for lipid nanoparticles [25] and tailored for the higher density of polymeric NPs like PLGA and PLA.
I. Principle: This method separates protein-NP complexes from unbound proteins and endogenous biological nanoparticles (e.g., exosomes, lipoproteins) based on their buoyant density using a continuous sucrose gradient. This avoids the aggregation and corona disruption associated with high-speed pelleting centrifugation [25].
II. Materials and Reagents:
- Polymeric Nanoparticles (e.g., PLGA, PLA, PACE), sterile
- Relevant Biological Fluid (e.g., human plasma, amniotic fluid)
- Ultracentrifuge and Swinging-Bucket Rotor
- Sucrose, Ultra-Pure
- PBS (Phosphate Buffered Saline), pH 7.4
- Liquid Chromatography-Mass Spectrometry (LC-MS/MS) system
III. Procedure:
- NP Incubation: Incubate a known concentration of PNPs (e.g., 1 mg/mL) with the biological fluid (e.g., 50% plasma in PBS) for a predetermined time (e.g., 1 hour) at 37°C with gentle agitation.
- Gradient Preparation: Prepare a continuous sucrose density gradient (e.g., 10-60% w/v in PBS) in ultracentrifuge tubes. Use a gradient maker for precise linearity.
- Sample Layering: Carefully layer the NP-biofluid incubation mixture on top of the pre-formed sucrose gradient.
- Ultracentrifugation: Centrifuge at approximately 160,000 × g for 16-24 hours at 4°C. This extended duration is critical for effective separation from endogenous particles [25].
- Fraction Collection: After centrifugation, carefully fractionate the gradient from the top. The protein-NP complexes will form a band at their buoyant density.
- Fraction Analysis: Analyze fractions for nanoparticle content (via fluorescence or absorbance) and protein content (e.g., BCA assay). Pool fractions rich in protein-NP complexes.
- Buffer Exchange and Washing: Use centrifugal filters (e.g., 100 kDa MWCO) to exchange the buffer into pure PBS or water and concentrate the samples. This step removes sucrose and loosely bound ("soft corona") proteins.
- Protein Elution and Identification:
- Denature the recovered complexes with Laemmli buffer.
- Analyze protein composition using SDS-PAGE for a general profile.
- For precise identification and quantification, digest the proteins with trypsin and analyze the peptides via LC-MS/MS.
Protocol: Evaluating Cellular Uptake of Corona-Coated Nanoparticles
I. Principle: This protocol assesses how the pre-formed PC influences the interaction of PNPs with target cells in vitro, providing a functional readout of the PC's biological activity.
II. Procedure:
- Prepare PC-Coated NPs: Generate PC-coated NPs using the isolation method above or a simplified incubation followed by buffer exchange to remove unbound proteins.
- Cell Seeding: Seed relevant cell lines (e.g., A549 for lung, Caco-2 for intestine) in multi-well plates and culture until ~80% confluent.
- NP Treatment: Treat cells with PC-coated NPs and pristine (non-coated) NPs at equal concentrations. Include a fluorescence label (e.g., DiD, Cy5) in the NP formulation for quantification.
- Incubation and Washing: Incubate for a set period (e.g., 2-4 hours) at 37°C. Subsequently, wash cells thoroughly with PBS to remove non-internalized NPs.
- Analysis:
- Flow Cytometry: Trypsinize and resuspend cells. Analyze cell-associated fluorescence using a flow cytometer to quantify the mean fluorescence intensity (MFI) per cell, which corresponds to NP uptake.
- Confocal Microscopy: Fix washed cells and stain nuclei and actin cytoskeleton. Use a confocal microscope to visually confirm internalization and subcellular localization of the fluorescent NPs.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for Protein Corona and Biodistribution Studies
| Reagent / Material | Function / Role in Research | Key Considerations |
|---|---|---|
| Biodegradable Polymers (PLGA, PLA, PACE) | Form the core matrix of the nanoparticle; determine biodegradability, cargo release kinetics, and initial surface properties for protein interaction. [19] [26] | PLGA is FDA-approved. PACE offers high nucleic acid encapsulation efficiency and tunable cytotoxicity. [19] |
| PEGylated Lipids / Polymers (e.g., PLGA-PEG) | Impart "stealth" properties by reducing opsonin adsorption, enhancing circulation time, and influencing PC composition. [19] [24] | PEG density is inversely correlated with total protein adsorption. High PEG density forms a brush conformation. [19] |
| Polyvinyl Alcohol (PVA) | Commonly used as a surfactant and stabilizer during nanoparticle formulation via emulsion. [19] | Residual PVA on the NP surface can influence subsequent protein corona formation and must be characterized. [19] |
| Apolipoproteins (ApoA1, ApoE) & Clusterin | Key "dysopsonins" (stealth proteins) in the corona. Pre-coating with these can actively engineer a stealth corona to reduce macrophage uptake. [22] [23] | Stability of pre-coated layers in full plasma is a key research challenge. Significant interspecies differences exist. [23] |
| Density Gradient Media (Sucrose, Iodixanol) | Enable gentle separation of protein-NP complexes from unbound proteins and endogenous particles for clean corona analysis. [25] | Critical for avoiding artifacts and obtaining a true representation of the hard corona composition. |
Visualization of the Protein Corona's Impact on Biodistribution
The following diagram synthesizes the critical steps and decision points that link nanoparticle properties to ultimate biodistribution through the mechanism of protein corona formation.
Diagram Title: How Protein Corona Determines Nanoparticle Fate In Vivo
The protein corona is not a confounding artifact but a fundamental determinant of the in vivo journey of polymeric nanoparticles. As demonstrated, its composition, governed by the NP's synthetic identity and biological environment, directly controls cellular interactions and biodistribution profiles. Moving forward, the field is transitioning from simply observing the PC to actively engineering it. Strategies include pre-coating NPs with specific "stealth" or "targeting" proteins like ApoA1 to dictate biological outcomes [23], and using Artificial Intelligence (AI) and Machine Learning (ML) to predict corona composition based on NP physicochemical parameters, thereby accelerating rational design [20]. Furthermore, leveraging the PC as a diagnostic tool by analyzing its "personalized" fingerprint in patient biofluids represents a promising frontier for disease detection [20]. For researchers, integrating robust PC characterization into the standard development workflow for polymeric nanoparticle drug delivery systems is no longer a niche activity but a critical step toward creating effective, targeted, and translatable nanomedicines.
In the development of polymeric nanoparticle (PNP) drug delivery systems, achieving targeted delivery and optimal therapeutic efficacy hinges on the precise engineering of physicochemical properties. Size, shape, and surface charge are fundamental design parameters that collectively govern the biological identity of nanoparticles, influencing their stability, circulation half-life, cellular uptake mechanisms, and biodistribution profiles [27] [28]. A deep understanding of the structure-function relationships dictated by these parameters is essential for advancing PNP-based strategies from laboratory research to clinical application. This document provides a detailed overview of these critical parameters, supported by quantitative data and standardized experimental protocols, to guide researchers in the rational design of polymeric nanocarriers.
Quantitative Analysis of Key Parameters
The following tables summarize the target ranges and biological implications of size, shape, and surface charge, as established by current research.
Table 1: Optimal Size Ranges for Different Biological Processes
| Biological Process | Optimal Size Range | Biological Implication & Rationale |
|---|---|---|
| Avoiding Renal Clearance | >10 nm [27] | Prevents rapid elimination through kidney filtration. |
| Reducing MPS/Uptake | ~150 nm [29] | Helps evade phagocytosis by the mononuclear phagocyte system. |
| Enhancing Cellular Uptake | ~50-100 nm [28] | Generally favorable for efficient cellular internalization. |
| Promoting EPR Effect | 10-200 nm [27] | Facilitates passive accumulation in tumor tissues through leaky vasculature. |
Table 2: Influence of Surface Charge on Biological Interactions
| Surface Charge (Zeta Potential) | Key Biological Interactions | Considerations for Design |
|---|---|---|
| Positive (Cationic) | Promotes strong electrostatic interaction with anionic cell membranes, generally leading to higher cellular uptake [29] [28]. | Can induce higher cytotoxicity and is more rapidly cleared from circulation by the immune system [27]. |
| Neutral | Minimizes non-specific interactions, leading to longer circulation times (e.g., via PEGylation) [27]. | May require functionalization with targeting ligands to achieve specific cellular uptake. |
| Negative (Anionic) | Can reduce protein opsonization compared to cationic surfaces but may still be recognized by specific serum proteins [27]. | A strongly negative charge may still lead to clearance by the MPS; a slightly negative to neutral charge (~-15 to 0 mV) is often optimal for longevity [29]. |
Table 3: Impact of Nanoparticle Shape on Delivery Efficacy
| Shape | Impact on Delivery and Biological Interactions |
|---|---|
| Spherical | The most commonly studied shape; cellular uptake is highly dependent on diameter [27]. |
| Rod / Cylindrical | Altered cellular internalization kinetics and circulation times compared to spheres [27]. |
| Other (Discoidal, etc.) | Different shapes can significantly influence margination, vascular transport, and phagocytosis [27]. |
Experimental Protocols for Parameter Control and Characterization
Protocol: Controlling Nanoparticle Size via Flash Nanoprecipitation
Principle: This flow-based method provides superior control over particle size and distribution by enabling rapid, homogeneous mixing, which leads to consistent nucleation and growth of polymeric nanoparticles [30].
Materials:
- Polymer: e.g., PEG--PLGA (Poly(lactic--co-glycolic acid))
- Organic Solvent: Water-miscible (e.g., Tetrahydrofuran, Acetone)
- Aqueous Solution: Deionized water or phosphate-buffered saline (PBS)
- Equipment: Syringe pumps, precision-bore tubing, mixing chamber, collection vessel
Procedure:
- Solution Preparation: Dissolve the polymer and hydrophobic drug (if applicable) in the organic solvent to form the organic phase.
- Apparatus Setup: Load the organic and aqueous phases into separate syringes mounted on syringe pumps. Connect the syringes to the inlets of a confined impingement jet (CIJ) or other multi-inlet vortex mixer.
- Mixing and NP Formation: Simultaneously drive the two streams at high velocity (typical total flow rate >10 mL/min) into the mixing chamber. The rapid and homogeneous mixing causes the polymer to supersaturate and precipitate, forming nanoparticles.
- Solvent Removal: Collect the effluent and stir gently to allow for the diffusion and removal of residual organic solvent.
- Purification: Purify the resulting nanoparticle suspension by dialysis or tangential flow filtration to remove solvents and unencapsulated cargo.
Notes: Particle size can be tuned by adjusting parameters such as polymer concentration, molecular weight, flow rate ratio, and total flow rate [30].
Protocol: Modifying Surface Charge and Coating
Principle: The surface charge (zeta potential) of PNPs is critical for their stability and interaction with biological components. Coating with hydrophilic polymers like PEG (polyethylene glycol) is a standard method to confer a neutral charge and "stealth" properties [27].
Materials:
- Pre-formed polymeric nanoparticles (e.g., from Protocol 3.1)
- PEG-lipid (e.g., DSPE-PEG) or other functionalized PEG polymers
- Phosphate Buffered Saline (PBS), pH 7.4
- Lab-scale stirrer/hot plate
Procedure:
- Post-Formation Coating: Add a solution of DSPE-PEG in PBS or another suitable buffer directly to the prepared nanoparticle suspension. A typical final PEG-lipid concentration is 0.1-1.0 mg/mL.
- Incubation: Incubate the mixture for 30-60 minutes at room temperature or a temperature above the phase transition of the lipid (e.g., 40-50°C) with gentle stirring.
- Purification: Purify the PEG-coated nanoparticles via dialysis, gel filtration, or centrifugation to remove unincorporated PEG-lipid.
- Verification: Measure the zeta potential of the nanoparticles before and after coating using dynamic light scattering (DLS). Successful PEGylation is indicated by a shift towards neutral potential (approximately 0 to -10 mV) and a potential reduction in polydispersity index.
Notes: Alternative coatings such as poly(2-oxazoline) (POx), polypeptides, or zwitterionic polymers can be explored to mitigate potential anti-PEG immunity [27].
Protocol: Characterizing Size, Surface Charge, and Morphology
Principle: A multi-technique approach is required to accurately characterize the physicochemical properties of PNPs, as each method provides complementary information [31].
Materials:
- Nanoparticle suspension
- Deionized water or appropriate buffer (for DLS/Zeta Potential)
- Filter membranes (e.g., 0.22 or 0.45 µm)
- Copper grids with carbon support film (for TEM)
- Staining solution (e.g., uranyl acetate)
Procedure:
- Dynamic Light Scattering (DLS) for Hydrodynamic Size:
- Dilute a small aliquot of the nanoparticle suspension in a clean, particle-free buffer to avoid scattering from dust or aggregates.
- Transfer to a disposable cuvette and measure the intensity-based size distribution and polydispersity index (PDI) using a DLS instrument. A PDI <0.2 is generally considered monodisperse.
Laser Doppler Electrophoresis for Zeta Potential:
- Dilute the nanoparticle sample in a low-conductivity buffer (e.g., 1 mM KCl) or a standard specified by the manufacturer.
- Load the sample into a folded capillary cell or appropriate cell.
- Measure the electrophoretic mobility and calculate the zeta potential using the Smoluchowski equation.
Electron Microscopy for Morphology and Actual Size:
- Sample Preparation: Place a small drop (5-10 µL) of diluted nanoparticle suspension onto a TEM grid. After 1-2 minutes, wick away the excess liquid with filter paper. Negative stain with 1-2% uranyl acetate for 30-60 seconds, then wick away the excess and allow the grid to air-dry completely.
- Imaging: Image the samples using Transmission Electron Microscopy (TEM) at appropriate accelerating voltages (e.g., 80-120 kV). TEM provides direct visualization of nanoparticle core size, shape, and morphology (e.g., spherical, cylindrical, vesicular) [31].
Visualization of Design Logic and Biological Fates
The following diagrams illustrate the logical framework for PNP design and the subsequent biological pathways they encounter.
Diagram 1: The interrelationship between key design parameters and the development pathway for polymeric nanoparticles.
Diagram 2: The influence of nanoparticle properties on key biological pathways post-administration. MPS: Mononuclear Phagocyte System; EPR: Enhanced Permeability and Retention.
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for PNP Development
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Biodegradable Polymers | The core structural material forming the nanoparticle matrix. | PLGA, PLA, PCL, Chitosan and its derivatives [29] [28]. |
| PEGylated Lipids/Polymers | Impart "stealth" properties to reduce opsonization and extend circulation half-life. | DSPE-PEG, PLGA--PEG block copolymers [27] [30]. |
| Fluorescent Dyes | Enable tracking and visualization of nanoparticles in in vitro and in vivo studies. | Rhodamine B (RhB), FITC, Coumarin-6 [29] [28]. |
| Characterization Tools | Essential for measuring the critical quality attributes (CQAs) of the final formulation. | DLS for size, Zeta Potential analyzer, TEM/SEM for morphology [31]. |
From Bench to Bedside: Fabrication Techniques and Therapeutic Applications
Polymeric nanoparticles (PNPs) are at the forefront of advancing drug delivery systems, offering unparalleled control over therapeutic agent release, enhanced targeting precision, and improved bioavailability [32]. The efficacy and application of these nanocarriers are profoundly influenced by their fabrication method, which dictates critical attributes such as particle size, morphology, drug loading efficiency, and release kinetics [33] [34]. This article details three core fabrication techniques—nanoprecipitation, emulsification, and ionic gelation—within the context of polymeric nanoparticle drug delivery research. It provides detailed application notes and standardized protocols to support scientists and drug development professionals in optimizing nanoparticle formulations for pre-clinical and clinical translation.
Nanoprecipitation
Principle and Applications
Nanoprecipitation, also termed solvent displacement or the "Ouzo effect," is a versatile and efficient technique for formulating PNPs [33] [34]. This method is based on the precipitation of a polymer and a hydrophobic drug from a water-miscible organic solution upon addition to an aqueous phase (anti-solvent) [35]. The process involves four key stages: supersaturation, nucleation, growth by condensation, and growth by coagulation, leading to the formation of a colloidal suspension of nanoparticles [35] [34]. Its advantages include simple methodology, minimal energy input, high reproducibility, and the general absence of surfactants, thereby reducing potential toxicity [33] [34]. Nanoprecipitation is suitable for encapsulating both hydrophobic and hydrophilic drugs and has been successfully applied for the controlled delivery of various therapeutic agents [35].
Critical Experimental Parameters
The properties of the resulting nanoparticles are highly dependent on several process and formulation parameters. Key factors include the polymer type and concentration, solvent and anti-solvent selection, organic-to-aqueous phase ratio, and the mixing method and kinetics [33] [35]. Rapid mixing, as achieved in flash (FNP) or microfluidic nanoprecipitation (MNP), provides superior control over particle size and distribution compared to conventional batch mixing [33] [34].
Table 1: Key Parameters in Nanoprecipitation Optimization
| Parameter | Impact on Nanoparticle Characteristics | Common Options / Optimal Range |
|---|---|---|
| Polymer Type | Determines biodegradability, drug compatibility, and release kinetics. | PLGA, PLA, PCL, PLA-PEG, chitosan [33] [34]. |
| Polymer Concentration | Influences particle size and drug loading capacity. | Typically 0.1 - 1% (w/v); must be optimized [34]. |
| Solvent Choice | Affects polymer solubility and rate of diffusion into anti-solvent. | Acetone, tetrahydrofuran (THF), ethanol [33] [35]. |
| Solvent-to-Anti-solvent Ratio | Impacts supersaturation level and final particle size. | Commonly 1:5 to 1:10 (organic:aqueous) [33]. |
| Mixing Method | Governs mixing time, homogeneity, and batch-to-batch consistency. | Batch (pipette/dropwise), Flash (FNP), Microfluidic (MNP) [33]. |
| Drug-to-Polymer Ratio | Critical for achieving high encapsulation efficiency. | Varies by drug-polymer system; requires experimental optimization [35]. |
Standardized Protocol for Batch Nanoprecipitation
Materials:
- Polymer (e.g., PLGA, 50 mg)
- Hydrophobic drug (e.g., 5 mg)
- Organic solvent, water-miscible (e.g., acetone, 10 mL)
- Aqueous anti-solvent (e.g., deionized water, 50 mL)
- Magnetic stirrer and stir bar
- Syringe and needle or pipette
Procedure:
- Organic Phase Preparation: Dissolve the polymer and the drug completely in the organic solvent to form a clear solution.
- Aqueous Phase Preparation: Place the aqueous anti-solvent (water) in a beaker under moderate magnetic stirring (500-600 rpm).
- Precipitation: Using a syringe or pipette, add the organic phase dropwise (e.g., at a rate of 0.5-1 mL/min) into the aqueous phase under constant stirring.
- Stirring: Continue stirring the resulting milky suspension for 3-4 hours at room temperature to allow for nanoparticle formation and evaporation of the organic solvent.
- Purification: Purify the nanoparticle suspension by centrifugation (e.g., 20,000 rpm for 30 minutes) and resuspend the pellet in distilled water or buffer for further analysis and use.
Diagram 1: Nanoprecipitation Workflow
Ionic Gelation
Principle and Applications
Ionic gelation is a mild, self-assembly process ideal for encapsulating hydrophilic drugs and sensitive biomolecules [36] [37]. This method relies on the electrostatic cross-linking between a charged polymer (polyelectrolyte) and an oppositely charged ion or polymer [37]. The most common system involves the cationic polysaccharide chitosan and the polyanion sodium tripolyphosphate (TPP) [36]. When mixed, the NH₃⁺ groups on chitosan form ionic linkages with the P₃O₁₀⁵⁻ groups of TPP, leading to the instantaneous gelation and formation of a nanoparticle network [36] [37]. The key advantages of this technique are its simplicity, execution in an aqueous environment, avoidance of organic solvents, and use of generally recognized as safe (GRAS) materials [36] [38].
Critical Experimental Parameters
The characteristics of chitosan-TPP nanoparticles are highly sensitive to synthesis conditions. A systematic optimization of the following parameters is crucial [36]:
Table 2: Key Parameters in Ionic Gelation Optimization
| Parameter | Impact on Nanoparticle Characteristics | Common Options / Optimal Range |
|---|---|---|
| Chitosan Parameters | ||
| - Molecular Weight | Affects viscosity, particle size, and gel density. | Low to medium molecular weight is often preferred. |
| - Degree of Deacetylation | Determines the number of available NH₃⁺ sites for cross-linking. | > 75% is typical [36]. |
| - Concentration | Higher concentrations can lead to larger particles or aggregation. | 0.1% - 0.5% (w/v) [36]. |
| Solution pH | Critically affects chitosan chain charge and expansion. | pH 4.6 - 5.5 is optimal for chitosan protonation [36]. |
| TPP Concentration | Impacts cross-linking density, particle size, and stability. | 0.1% - 0.5% (w/v); Chitosan:TPP mass ratio of ~3:1 to 5:1 [36]. |
| Mixing Conditions | ||
| - Stirring Speed | Influences mixing homogeneity and particle size. | 500 - 700 rpm [36]. |
| - Addition Time (Dripping) | Affects the rate of cross-linking and particle uniformity. | 2 - 6 minutes for 1.7 mL of TPP solution [36]. |
Standardized Protocol for Chitosan-TPP Nanoparticle Synthesis
Materials:
- Chitosan (low molecular weight, 75-85% deacetylation)
- Sodium Tripolyphosphate (TPP)
- Acetic acid (1% v/v)
- Sodium hydroxide (NaOH, 20% solution for pH adjustment)
- Magnetic stirrer
- Syringe and needle or peristaltic pump
Procedure:
- Chitosan Solution Preparation: Dissolve chitosan in 1% acetic acid solution to a final concentration of 0.1% (w/v). Adjust the pH of the solution to 5.5 using 20% NaOH. Filter the solution through a 0.22 µm membrane.
- TPP Solution Preparation: Dissolve TPP in deionized water to a concentration of 0.1% (w/v).
- Cross-linking and Nanoparticle Formation: Under constant magnetic stirring at 500 rpm, add 1.7 mL of the TPP solution dropwise (e.g., over 2 minutes) into 5 mL of the chitosan solution.
- Stirring: Continue stirring the suspension for 30 minutes at room temperature to allow for nanoparticle hardening.
- Purification and Stabilization: Purify the nanoparticles by centrifugation or dialysis. To enhance stability during purification and storage, surfactants like Poloxamer 188 or Polysorbate 80 (1% w/v) can be added [36]. For long-term storage, freeze-drying with cryoprotectants like trehalose or sucrose (5-10% w/v) is recommended [36].
Diagram 2: Ionic Gelation Workflow
Emulsification-Solvent Evaporation
Principle and Applications
The emulsification-solvent evaporation method is a widely used technique for encapsulating hydrophobic drugs [39]. The process involves two primary steps: first, the formation of a primary emulsion, where a polymer and drug dissolved in a water-immiscible organic solvent (e.g., dichloromethane or ethyl acetate) is emulsified in an aqueous phase containing a stabilizer (emulsifier) to form an oil-in-water (O/W) emulsion [39] [40]. Second, the organic solvent is evaporated under reduced pressure or stirring, leading to the precipitation of the polymer and the formation of solid nanoparticles [39]. The method provides high encapsulation efficiencies for lipophilic compounds and allows for control over particle size through homogenization energy [40].
Critical Experimental Parameters
The stability and characteristics of the nanoemulsion and final nanoparticles are governed by several factors [39] [40]:
Table 3: Key Parameters in Emulsification-Solvent Evaporation Optimization
| Parameter | Impact on Nanoparticle Characteristics | Common Options / Optimal Range |
|---|---|---|
| Oil-to-Water Phase Ratio | Influences emulsion type and droplet size. | Varies; a small organic phase volume is typical for O/W emulsions. |
| Emulsifier/Stabilizer Type & Concentration | Critical for preventing droplet coalescence and ensuring colloidal stability. | Polyvinyl alcohol (PVA), polysorbates, poloxamers, caseinates [39] [40]. |
| Homogenization Method & Energy | Directly determines the droplet and final particle size. | High-speed homogenization (e.g., 2,000-10,000 rpm) or ultrasonication [39]. |
| Solvent Removal Rate | Affects particle morphology and drug distribution. | Stirring at room pressure or under reduced pressure. |
| Environmental Stresses (pH, T, electrolytes) | Can destabilize the emulsion; parameters must be optimized for stability [39]. | Alkaline pH (e.g., 9), temperatures up to 50°C, electrolyte concentrations up to 100 mM may be tolerated in optimized systems [39]. |
Standardized Protocol for O/W Nanoemulsion Formation
Materials:
- Polymer (e.g., PLGA, 100 mg)
- Hydrophobic drug (e.g., 10 mg)
- Organic solvent, water-immiscible (e.g., dichloromethane, 10 mL)
- Emulsifier (e.g., Polyvinyl Alcohol - PVA, 1-2% w/v solution)
- High-speed homogenizer or ultrasonic probe
- Magnetic stirrer and stir bar
Procedure:
- Organic Phase Preparation: Dissolve the polymer and drug in the water-immiscible organic solvent.
- Aqueous Phase Preparation: Prepare an aqueous solution of the emulsifier (e.g., 1% PVA in water).
- Primary Emulsion Formation: Add the organic phase to the aqueous phase. Immediately homogenize the mixture using a high-speed homogenizer (e.g., 10,000 rpm for 5 minutes) or an ultrasonic probe to form a coarse O/W emulsion.
- Size Reduction: Further reduce the droplet size by sonication (e.g., on an ice bath for 1-2 minutes at a specific power output) to form a nanoemulsion.
- Solvent Evaporation: Stir the nanoemulsion continuously at room temperature for several hours (or under reduced pressure) to evaporate the organic solvent, solidifying the nanoparticles.
- Purification: Collect the nanoparticles by ultracentrifugation, wash repeatedly with water to remove excess emulsifier, and resuspend for analysis.
Diagram 3: Emulsification-Solvent Evaporation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Polymeric Nanoparticle Fabrication
| Reagent Category | Specific Examples | Function in Formulation |
|---|---|---|
| Biodegradable Polymers | Poly(lactic-co-glycolic acid) (PLGA), Poly(lactic acid) (PLA), Poly(ε-caprolactone) (PCL) [33] [34] | Forms the nanoparticle matrix; determines biodegradability, drug release profile, and biocompatibility. |
| Natural Polyelectrolytes | Chitosan, Sodium Alginate, Hyaluronic Acid [36] [37] [38] | Acts as the primary gelling or structural polymer in ionic gelation; offers mucoadhesion and mild processing. |
| Cross-linking Agents | Sodium Tripolyphosphate (TPP), Calcium Chloride (CaCl₂) [36] [37] | Induces ionic gelation by forming bridges between polyelectrolyte chains to create a nanoparticle network. |
| Emulsifiers & Stabilizers | Polyvinyl Alcohol (PVA), Poloxamer 188, Polysorbate 80, Sodium Caseinate [36] [39] [40] | Reduces interfacial tension during emulsification; prevents aggregation and stabilizes the formed nanoparticles. |
| Cryoprotectants | Trehalose, Sucrose [36] | Protects nanoparticle structure from ice crystal damage and prevents aggregation during freeze-drying for long-term storage. |
In the development of polymeric nanoparticle (PNP) drug delivery systems, advanced characterization of size, stability, and drug release profiles is paramount for ensuring therapeutic efficacy and successful clinical translation [6]. These physicochemical parameters directly influence critical biological interactions, including biodistribution, cellular uptake mechanisms, and controlled release kinetics at target sites [41] [42]. This document provides detailed application notes and standardized protocols to enable researchers to obtain reliable, reproducible characterization data that can effectively guide PNP formulation optimization.
The characterization process presents significant challenges due to the nanoscale dimensions and dynamic behavior of PNPs in complex biological environments [42]. No single technique provides a complete picture; instead, a complementary, orthogonal approach combining multiple methodologies is essential for comprehensive understanding [43]. The following sections outline standardized methodologies and data interpretation frameworks to address these challenges systematically.
Particle Size and Size Distribution Analysis
Orthogonal Technique Approach
Particle size directly impacts PNPs' in vivo behavior, including circulation time, tissue penetration, and cellular internalization. Employing orthogonal techniques provides a more comprehensive understanding of PNP size distributions than any single method could achieve independently [43].
Table 1: Comparison of Primary Sizing Techniques for Polymeric Nanoparticles
| Technique | Size Range | Principle | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Dynamic Light Scattering (DLS) | 1 nm - 6 μm | Measures Brownian motion to calculate hydrodynamic diameter | Rapid analysis, high sensitivity to large aggregates, minimal sample preparation [41] [43] | Intensity-weighted distribution biased toward larger particles, assumes spherical morphology [41] |
| Nanoparticle Tracking Analysis (NTA) | 10 - 2000 nm | Tracks and analyzes individual particle movement | Direct visualization, provides concentration data, superior for polydisperse samples [41] | Lower concentration range, analysis time longer than DLS [41] |
| Transmission Electron Microscopy (TEM) | <1 nm - μm | High-resolution electron imaging | Ultimate size and morphological detail, reveals structural heterogeneity [41] [42] | Vacuum conditions may alter samples, dry-state measurement, complex sample preparation [41] |
Step-by-Step Protocol for Multi-Technique Sizing
Protocol Title: Comprehensive Size Analysis of Polymeric Nanoparticles Using Orthogonal Techniques
Principle: This protocol leverages the complementary strengths of DLS, NTA, and TEM to obtain a complete understanding of PNP size distribution and morphology [41] [43].
Materials:
- Purified PNP suspension (e.g., PLGA, chitosan-based systems)
- Dialysis buffer (e.g., phosphate-buffered saline, pH 7.4)
- Filtered, deionized water (0.02 μm filtered)
- TEM grids (e.g., copper grids with carbon support film)
- Negative stain (e.g., 2% uranyl acetate)
- DLS instrument (e.g., Malvern Zetasizer)
- NTA instrument (e.g., Malvern NanoSight)
- TEM instrument
Procedure:
- Sample Preparation:
- Dialyze PNP suspensions against an appropriate buffer to remove free polymer and surfactants.
- Prepare three dilutions of the sample in filtered buffer (typically 1:10 to 1:100) to identify optimal concentration ranges for each instrument.
Dynamic Light Scattering:
- Transfer 1 mL of appropriately diluted sample into a disposable sizing cuvette.
- Equilibrate to measurement temperature (typically 25°C or 37°C) for 300 seconds.
- Perform minimum of 12 measurements per sample with automatic attenuation selection.
- Record intensity-weighted size distribution, polydispersity index (PdI), and cumulants mean (Z-average).
Nanoparticle Tracking Analysis:
- Load diluted sample via sterile syringe, ensuring careful exclusion of air bubbles.
- Capture five 60-second videos at camera level 14-16, ensuring particle count between 20-100 particles/frame.
- Process all videos with identical detection threshold and screen gain settings.
- Report mode and mean size from number-weighted size distribution.
Transmission Electron Microscopy:
- Glow-discharge TEM grids to enhance hydrophilicity.
- Apply 5 μL of sample to grid, incubate 60 seconds, blot excess with filter paper.
- Wash with 5 μL filtered water, blot immediately.
- Stain with 5 μL uranyl acetate (2%) for 30 seconds, blot thoroughly.
- Image at multiple magnifications (e.g., 10,000x to 50,000x) across grid squares.
Data Interpretation Guidelines:
- Compare DLS (intensity-weighted) and NTA (number-weighted) distributions to identify presence of aggregates or subpopulations [41].
- Use TEM data to validate size measurements and provide critical information on particle morphology and structural homogeneity [42].
- Significant discrepancies between DLS and NTA often indicate sample polydispersity requiring formulation optimization.
Stability Assessment Under Physiological Conditions
Critical Stability Parameters
PNP stability extends beyond shelf-life to encompass performance in biologically relevant environments. Key parameters include colloidal stability (resistance to aggregation), structural integrity under physiological conditions, and interaction with biological components [43].
Table 2: Key Stability Parameters and Assessment Methodologies
| Stability Parameter | Assessment Technique | Experimental Conditions | Acceptance Criteria |
|---|---|---|---|
| Colloidal Stability | DLS (size and PDI), Zeta Potential | Storage in formulation buffer (4°C, 25°C), freeze-thaw cycling | Size change < 10%, PDI < 0.2, zeta potential change < 5 mV |
| Serum Stability | DLS, NTA, Fluorescence Correlation Spectroscopy | Incubation in 10-50% FBS/PBS at 37°C with gentle agitation | Limited size increase, no macroscopic aggregation |
| Storage Stability | DLS, HPLC (drug content), Visual Inspection | Accelerated stability (4°C, 25°C, 40°C) over 1-6 months | Maintains physicochemical properties, no precipitation |
Protocol for Serum Stability Assessment
Protocol Title: Evaluation of Polymeric Nanoparticle Stability in Biological Media
Principle: This protocol assesses the stability of PNPs upon exposure to biologically relevant media, simulating in vivo conditions and predicting performance upon administration [43].
Materials:
- PNP suspension (1-10 mg/mL in PBS)
- Fetal bovine serum (FBS) or human serum
- Incubator/shaker maintaining 37°C
- DLS instrument
- NTA instrument
- Centrifugal filters (100 kDa MWCO)
Procedure:
- Sample Preparation:
- Pre-warm serum to 37°C in water bath.
- Mix PNP suspension with serum to achieve final concentrations of 10%, 25%, and 50% serum (v/v).
- Prepare control samples in PBS alone.
Time-Course Measurements:
- Incubate serum-PNP mixtures at 37°C with gentle agitation (50-100 rpm).
- Withdraw aliquots (50 μL) at predetermined time points (0, 0.5, 1, 2, 4, 8, 24 hours).
- For DLS analysis, dilute samples 1:10 in corresponding serum-PBS mixture to maintain constant scattering background.
- For NTA analysis, dilute samples 1:100-1:1000 in filtered PBS to achieve optimal particle density.
Data Collection:
- Perform DLS measurements in triplicate at each time point.
- Capture three 60-second NTA videos per time point.
- Centrifuge select samples through 100 kDa filters at 14,000 × g for 45 minutes to separate released drug for quantification by HPLC.
Interpretation and Analysis:
- Plot hydrodynamic diameter, PDI, and particle concentration versus time.
- Significant increases in size indicate aggregation or protein corona formation.
- Decreasing particle concentration suggests dissolution or extensive aggregation beyond detection limits.
- Correlation of physical stability with drug release profiles provides insights into formulation robustness.
Drug Release Kinetics Profiling
Methodological Considerations
Accurate characterization of drug release profiles is essential for predicting in vivo performance but presents significant technical challenges. Traditional methods like dialysis membrane (DM) approaches may misestimate release kinetics due to inadequate separation or additional diffusion barriers [44].
Table 3: Comparison of In Vitro Release Study Methods for Polymeric Nanoparticles
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| Dialysis Membrane (DM) | Separation of free drug through semi-permeable membrane | Simple setup, widely used | Potential underestimation of burst release, membrane adsorption issues, additional diffusion barrier [44] |
| Sample and Separate with Centrifugal Ultrafiltration (SS+CU) | Physical separation via centrifugal filtration | Direct measurement of free drug concentration, maintains sink conditions, no additional barriers [44] | Requires validation of separation efficiency, potential for continued release during separation |
| Continuous Flow (CF) | Continuous replacement of release medium | Maintains perfect sink conditions | Complex setup, low throughput, potential for particle loss [44] |
Recent investigations demonstrate that the Sample and Separate method with Centrifugal Ultrafiltration (SS+CU), when combined with USP apparatus II (paddle), provides superior accuracy and reproducibility for characterizing drug release from PNPs [44].
Advanced Protocol for Drug Release Studies
Protocol Title: Sample and Separate Method with Centrifugal Ultrafiltration for Drug Release Profiling
Principle: This protocol utilizes centrifugal ultrafiltration to efficiently separate released drug from nanoparticles during time-course studies, providing accurate release kinetics without the additional diffusion barrier of dialysis membranes [44].
Materials:
- USP Apparatus II (paddle apparatus)
- Centrifugal ultrafiltration devices (e.g., Amicon Ultra, 100 kDa MWCO)
- Release medium (e.g., PBS with 0.1-0.5% w/v SDS to maintain sink conditions)
- Water bath maintaining 37°C
- HPLC system with appropriate column and detection
Procedure:
- Sink Condition Validation:
- Determine drug solubility in selected release medium.
- Ensure medium volume is at least 3 times that required to form a saturated solution.
Release Study Setup:
- Place 500 μL of PNP suspension (or equivalent of 1-5 mg drug) into 100 mL release medium in USP apparatus II vessels.
- Maintain temperature at 37°C ± 0.5°C with paddle rotation at 50 rpm.
- At predetermined time intervals, withdraw 500 μL aliquots from each vessel.
Separation and Analysis:
- Immediately transfer aliquots to pre-rinsed centrifugal ultrafiltration devices.
- Centrifuge at 14,000 × g for 10 minutes at controlled temperature (37°C).
- Collect filtrate and analyze drug concentration using validated HPLC-UV method.
- Replace medium in vessels with equal volume of fresh pre-warmed medium to maintain constant volume.
Data Processing:
- Calculate cumulative drug release using standard equations accounting for sample removal.
- Plot cumulative release versus time to generate release profiles.
- Fit data to appropriate mathematical models (e.g., zero-order, first-order, Higuchi, Korsmeyer-Peppas) to elucidate release mechanisms.
Validation Parameters:
- Separation Efficiency: Confirm >98% nanoparticle retention in ultrafiltration device using DLS analysis of retentate.
- Non-specific Binding: Demonstrate <5% drug adsorption to filtration membrane.
- Stability: Verify drug stability in release medium over experiment duration.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for PNP Characterization
| Category | Specific Items | Function/Application | Examples/Notes |
|---|---|---|---|
| Polymer Systems | PLGA, Chitosan, HPMA, Poly(lactic acid) | PNP matrix materials providing structural framework and controlling release kinetics | Select based on biodegradability, biocompatibility, and regulatory status [6] [45] |
| Stabilizers | TPGS, PVA, Poloxamers | Prevent nanoparticle aggregation during formation and storage | TPGS particularly effective for flash nanoprecipitation [44] |
| Characterization Standards | Latex/nanosphere size standards, Buffer components | Instrument calibration and method validation | Essential for data comparability across laboratories [43] |
| Separation Materials | Centrifugal filters (10-100 kDa MWCO), Dialysis membranes | Separation of free drug from nanoparticles in release studies | 100 kDa MWCO typically effective for polymeric nanoparticles [44] |
| Analytical Tools | HPLC systems, DLS instruments, TEM grids | Quantification and morphological characterization | Orthogonal approach recommended [41] [43] [44] |
Advanced characterization of polymeric nanoparticles through robust, standardized protocols for size, stability, and drug release profiling is fundamental to rational formulation design and successful clinical translation. The orthogonal approach outlined in this document, combining multiple analytical techniques, provides a comprehensive framework for obtaining reliable data that accurately predicts PNP performance in vivo.
As the field progresses toward increasingly sophisticated "smart" delivery systems with stimuli-responsive capabilities [6], these fundamental characterization principles will remain essential for correlating material properties with biological performance. Implementation of these protocols will enhance data reproducibility and accelerate the development of effective polymeric nanoparticle-based therapeutics.
Within drug delivery systems, polymeric nanoparticles (PNPs) have emerged as a groundbreaking advancement for enabling targeted therapy. Their versatility, biocompatibility, and ability to encapsulate diverse therapeutic agents allow for controlled drug release, which improves efficacy while minimizing systemic side effects [12] [6]. The strategic delivery of these nanocarriers to diseased tissues primarily relies on two fundamental mechanisms: passive and active targeting. Passive targeting leverages the distinctive pathophysiological characteristics of diseased tissues, such as solid tumors, through the Enhanced Permeability and Retention (EPR) effect. In contrast, active targeting involves the functionalization of the nanoparticle surface with specific ligands (e.g., antibodies, peptides, folates) that recognize and bind to receptors overexpressed on target cells [12] [46]. This document provides detailed application notes and experimental protocols for leveraging these strategies within research on polymeric nanoparticle-based drug delivery systems.
Passive Targeting: The Enhanced Permeability and Retention (EPR) Effect
Mechanism and Theoretical Foundation
The EPR effect is a pathophysiological phenomenon first described in the 1980s, which facilitates the passive accumulation of macromolecules and nanoparticles in solid tumors [47]. This process is driven by the unique anatomical and physiological abnormalities of tumor vasculature and the surrounding microenvironment, which are highly heterogeneous [48] [47].
The core mechanisms underpinning the EPR effect include:
- Vascular Hyperpermeability: Tumor blood vessels are often abnormal, with poorly aligned, leaky endothelial cells and large inter-endothelial gaps ranging from 100 to 780 nm. This allows nanoparticles within a specific size range to extravasate from the bloodstream into the tumor interstitium [47].
- Impaired Lymphatic Drainage: Tumors frequently exhibit defective or absent lymphatic drainage systems. This failure in clearance leads to the prolonged retention of accumulated nanoparticles and macromolecules within the tumor tissue [47].
- The Tumor Microenvironment (TME): Factors such as high interstitial fluid pressure (IFP), a dense extracellular matrix (ECM), and the presence of inflammatory mediators like vascular endothelial growth factor (VEGF) and bradykinin sustain the EPR effect but also create barriers to uniform drug distribution [47].
The following diagram illustrates the key components and process of the EPR effect:
Quantitative Design Parameters for Exploiting the EPR Effect
The efficacy of passive targeting is critically dependent on the physicochemical properties of the polymeric nanoparticle. Optimizing these parameters is essential for maximizing circulation time, tumor accumulation, and therapeutic outcomes.
Table 1: Key Nanoparticle Physicochemical Properties for Passive Targeting via the EPR Effect
| Property | Optimal Range for EPR | Impact on Delivery Efficacy |
|---|---|---|
| Size | 10 - 200 nm [46] [49] | Particles <10 nm are rapidly cleared by renal filtration. Particles >200 nm are often sequestered by the spleen and liver (reticuloendothelial system, RES). The 10-200 nm range optimizes vascular extravasation and circulation time. |
| Surface Charge | Near-neutral or slightly negative [47] | Positively charged particles exhibit higher non-specific cellular uptake and faster clearance. Neutral/negative surfaces reduce opsonization and RES uptake, prolonging circulation. |
| Surface Hydrophilicity | Hydrophilic (e.g., via PEGylation) [12] [47] | Surface modification with hydrophilic polymers like polyethylene glycol (PEG) creates a "stealth" effect, reducing protein adsorption (opsonization) and recognition by macrophages. |
| Shape | Spherical or other low-aspect-ratio shapes [47] | The shape influences flow dynamics, margination toward vessel walls, and ability to traverse endothelial gaps. |
Protocol: Formulating PEGylated PLGA Nanoparticles for Passive Targeting
This protocol details the synthesis of poly(lactic-co-glycolic acid)-polyethylene glycol (PLGA-PEG) nanoparticles using the nanoprecipitation method, a standard technique for producing nanocarriers suitable for exploiting the EPR effect [49].
Research Reagent Solutions:
- Polymer: PLGA-PEG copolymer (e.g., PLGA-PEG-COOH, 50:50 monomer ratio, MW 10-30 kDa).
- Organic Solvent: Acetone (HPLC grade).
- Aqueous Phase: Deionized water or phosphate-buffered saline (PBS, 0.01 M, pH 7.4).
- Therapeutic Agent: Drug of choice (e.g., Doxorubicin hydrochloride).
Procedure:
- Organic Phase Preparation: Dissolve 50 mg of PLGA-PEG copolymer and 5 mg of the drug (for drug-loaded NPs) in 10 mL of acetone. Stir magnetically until the polymer and drug are completely dissolved.
- Aqueous Phase Preparation: Pour 20 mL of deionized water into a 50 mL beaker under gentle magnetic stirring (500-600 rpm).
- Nanoprecipitation: Using a glass syringe, add the organic phase dropwise (e.g., 1 mL/min) into the aqueous phase. The formation of a milky, opalescent suspension indicates nanoparticle self-assembly.
- Organic Solvent Removal: Place the nanoparticle suspension in a fume hood under constant stirring for 4-6 hours to allow for the complete evaporation of acetone. Alternatively, use rotary evaporation under reduced pressure.
- Purification and Concentration: Centrifuge the suspension at a mild speed (e.g., 5,000 x g for 10 minutes) to remove any large aggregates. Then, purify the supernatant via ultrafiltration (e.g., using a 100 kDa MWCO membrane) or dialysis (against deionized water for 2 hours) to remove free, unencapsulated drug and solvent traces.
- Characterization:
- Size and Zeta Potential: Dilute the purified NP suspension 1:10 in distilled water and analyze using Dynamic Light Scattering (DLS) and Laser Doppler Velocimetry. Target a hydrodynamic diameter of 80-150 nm and a zeta potential of -10 to -30 mV.
- Drug Loading and Encapsulation Efficiency: Lyophilize a known volume of the NP suspension. Dissolve the lyophilized powder in DMSO and quantify the drug content using UV-Vis spectroscopy or HPLC against a standard calibration curve.
Active Targeting: Ligand-Functionalized Polymeric Nanoparticles
Mechanism and Ligand Selection
Active targeting enhances the specificity of polymeric nanoparticles by decorating their surface with targeting ligands. These ligands bind to antigens or receptors that are overexpressed on the surface of target cells, such as cancer cells, promoting receptor-mediated endocytosis and increasing cellular uptake [12] [46]. This strategy can complement the EPR effect by ensuring that nanoparticles accumulated in the tumor vicinity are internalized by the correct cells, thereby minimizing off-target effects.
Common classes of targeting ligands include:
- Antibodies and Antibody Fragments: High specificity and affinity.
- Peptides: e.g., RGD peptide for targeting integrin receptors.
- Vitamins: e.g., Folic acid (Fol) for targeting folate receptors, which are overexpressed in many cancer cells [12] [49].
- Aptamers: Short, single-stranded DNA or RNA molecules.
The following diagram outlines the general workflow for developing and evaluating ligand-functionalized nanoparticles:
Protocol: Conjugating Folic Acid to PLGA Nanoparticles for Active Targeting
This protocol describes the covalent conjugation of folic acid (Fol) to amine-functionalized PLGA-PEG-NH₂ nanoparticles, creating a system for actively targeting folate receptor-positive cancer cells [12] [49].
Research Reagent Solutions:
- Nanoparticles: Pre-formed PLGA-PEG-NH₂ nanoparticles (synthesized via nanoprecipitation, as in Protocol 2.3).
- Ligand: Folic Acid (Fol).
- Coupling Agents: N-Hydroxysuccinimide (NHS) and N-(3-Dimethylaminopropyl)-N'-ethylcarbodiimide hydrochloride (EDC).
- Activation Buffer: MES buffer (0.1 M, pH 5.5).
- Purification Medium: Phosphate Buffered Saline (PBS, 0.01 M, pH 7.4).
Procedure:
- Ligand Activation:
- Dissolve 5 mg of folic acid in 2 mL of MES buffer.
- Add 7.5 mg of EDC and 4.5 mg of NHS to the folate solution.
- Activate the reaction by stirring for 15-30 minutes at room temperature in the dark. This step forms an NHS-ester intermediate of folic acid.
Ligand Conjugation:
- Add the activated folate solution dropwise to 10 mL of the PLGA-PEG-NH₂ nanoparticle suspension (~10 mg/mL in MES or PBS).
- Allow the conjugation reaction to proceed for 4-6 hours under constant stirring at room temperature, protected from light.
Purification:
- Transfer the reaction mixture to a dialysis membrane (MWCO 50-100 kDa).
- Dialyze against PBS (pH 7.4) for 24 hours with 3-4 buffer changes to remove unreacted EDC, NHS, and folic acid.
- Alternatively, purify using size-exclusion chromatography (e.g., Sephadex G-25 column).
Characterization and Validation:
- Confirming Conjugation: Use ( ^1 \text{H} ) Nuclear Magnetic Resonance (NMR) spectroscopy in D₂O/DMSO-d₆ to confirm the presence of characteristic folate peaks on the nanoparticle spectrum [31].
- Cellular Uptake Studies: Incubate folate-functionalized NPs (Fol-PNPs) and non-functionalized (control) PNPs with folate receptor-positive (e.g., MCF-7) and receptor-negative cell lines. Quantify uptake using flow cytometry or confocal microscopy (if NPs are fluorescently labeled). A significant increase in uptake for Fol-PNPs in receptor-positive cells confirms active targeting.
- Cytotoxicity Assay: Perform an MTT assay to compare the cytotoxicity of drug-loaded Fol-PNPs against control NPs. Enhanced cytotoxicity in target cells demonstrates improved therapeutic efficacy of the actively targeted system.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Developing Targeted Polymeric Nanoparticles
| Reagent / Material | Function / Role in Research | Examples & Notes |
|---|---|---|
| Biodegradable Polymers | Form the nanoparticle matrix; control degradation and drug release kinetics. | PLGA, PLA, PCL, Chitosan [46] [50]. PLGA is FDA-approved and widely used. |
| Stealth Polymers | Impart "stealth" properties to reduce immune clearance and prolong circulation. | PEG (PEGylation) is the gold standard. Alternatives include HPMA [12] [46]. |
| Targeting Ligands | Mediate specific binding to cellular receptors for active targeting. | Folic Acid [12], Peptides (e.g., RGD) [12], Antibodies (e.g., anti-P-glycoprotein) [12]. |
| Coupling Agents | Facilitate covalent conjugation of ligands to the nanoparticle surface. | EDC/NHS chemistry is most common for carboxyl-amine coupling [49]. |
| Characterization Instruments | Analyze physicochemical properties critical for targeting efficacy. | DLS (size, PDI), Zeta Potential Analyzer (surface charge), NMR, HPLC (drug loading) [31]. |
Passive targeting via the EPR effect and active targeting via ligand functionalization are complementary cornerstones of modern drug delivery using polymeric nanoparticles. While the EPR effect provides a foundational mechanism for initial tumor accumulation, its heterogeneity in human patients limits its reliability [48] [47]. Active targeting strategies are designed to overcome this limitation by enhancing specific cellular uptake and retention. The successful implementation of these strategies requires meticulous design and optimization of nanoparticle parameters, as outlined in the provided protocols and tables. Future perspectives in the field point towards the development of multi-stage, "smart" stimuli-responsive systems that can dynamically interact with the complex tumor microenvironment [12] [51], ultimately paving the way for more effective and personalized nanomedicines.
Polymeric nanoparticles (PNPs) represent a groundbreaking advancement in targeted drug delivery for oncology, offering significant benefits over conventional therapeutic systems. These nanoscale particles, typically ranging from 10 to 1000 nanometers, are engineered to encapsulate diverse therapeutic agents and provide controlled release, thereby improving therapeutic efficacy while minimizing side effects [31]. Their versatility, biocompatibility, and ability to navigate biological barriers make them particularly valuable for cancer immunotherapy applications [12]. The strategic design of PNPs enables enhanced drug delivery to tumor sites through both passive and active targeting mechanisms. Passive targeting leverages the Enhanced Permeability and Retention (EPR) effect, which exploits the leaky vasculature and impaired lymphatic drainage of tumor tissues to allow selective accumulation of nanoparticles [52]. Active targeting involves functionalizing the PNP surface with ligands such as antibodies, peptides, folates, or transferrin that specifically bind to receptors overexpressed on cancer cells or immune cells within the tumor microenvironment [12] [52]. This targeted approach is revolutionizing cancer treatment by enabling precise delivery of immunotherapeutic agents while reducing off-target effects.
Key Advantages of PNPs in Cancer Immunotherapy
Polymeric nanoparticles offer several distinct advantages that make them ideally suited for oncology and cancer immunotherapy applications:
Enhanced Bioavailability and Stability: PNPs protect therapeutic agents such as peptides, proteins, mRNAs, and small molecules from premature degradation, maintaining their bioactivity until they reach the target site [31] [17]. This is particularly valuable for labile immunotherapeutic agents that would otherwise be rapidly cleared from circulation.
Stimuli-Responsive Drug Release: Smart PNPs can be engineered to respond to specific stimuli in the tumor microenvironment, such as pH changes, temperature variations, or enzyme activity, enabling precise drug release at the desired site of action [12]. This controlled release profile improves therapeutic outcomes while minimizing systemic exposure.
Co-delivery Capabilities: PNPs can simultaneously deliver multiple therapeutic agents, such as combining chemotherapeutic drugs with immunomodulators or efflux pump inhibitors, to overcome multidrug resistance (MDR) and enhance anti-cancer efficacy [12] [52]. This combination approach is particularly promising for addressing the complex resistance mechanisms in cancer therapy.
Immune Cell Targeting: Surface-functionalized PNPs can specifically target immune cells such as dendritic cells, T cells, or antigen-presenting cells to modulate immune responses and enhance antitumor immunity [52] [53]. This precise targeting capability makes them valuable vehicles for next-generation cancer immunotherapies.
Quantitative Data on PNP Applications in Oncology
Table 1: Polymeric Nanoparticle Formulations for Cancer Therapy
| Polymer System | Loaded Agent | Cancer Type | Key Findings | Reference |
|---|---|---|---|---|
| PLGA-PEG | Paclitaxel | Breast, Pancreatic, Ovarian, Brain | Enhanced tumor targeting and reduced side effects | [54] |
| PCL-PEG-PCL | Paclitaxel | Lung | Effective in chrono-modulated chemotherapy | [54] |
| HPMA Copolymer | Pirarubicin | Solid Tumors | Superior penetration in tumor spheroids via EPR effect | [12] |
| Fol/R7 Nanoparticles | Docetaxel & Perifosine | Drug-resistant | Regulated PI3K/Akt pathway; increased cytotoxicity & apoptosis | [12] |
| Anti-P-gp Conjugated NPs | Various chemotherapeutics | Multi-drug resistant | Overcame resistance mechanisms; enhanced cellular uptake | [12] |
Table 2: PNP Formulations to Overcome Cancer Resistance Mechanisms
| Resistance Mechanism | PNP Approach | Therapeutic Outcome | Reference |
|---|---|---|---|
| Hypoxic Microenvironment | A-MnO₂ NPs generating O₂ | Increased pH from 6.7 to 7.2; attenuated hypoxia | [52] |
| HIF-1α overexpression | siRNA-loaded TAT-chitosan-SPION | Reduced HIF-1α & CD73 expression by >75% | [52] |
| P-glycoprotein Efflux | miR495 with silica NPs | Decreased MDR in A549/DOX cells to 38.5% vs 80% with free DOX | [52] |
| COX-2 mediated resistance | COX-2 inhibitor + DOX co-delivery | Significant tumor reduction; decreased COX-2 & P-gp expression <0.5 | [52] |
Experimental Protocols for PNP Development
PNP Fabrication Method: Solvent Evaporation
Principle: This method involves the formation of an oil-in-water (o/w) emulsion where the polymer is dissolved in an organic phase containing the drug, followed by evaporation of the solvent to form solid nanoparticles [54].
Step-by-Step Protocol:
- Organic Phase Preparation: Dissolve 100-500 mg of polymer (e.g., PLGA, PCL) in 10-20 mL of organic solvent (ethyl acetate recommended due to better toxicological profile). Add the drug compound (typically 10-20% w/w of polymer) to the organic phase with stirring until complete dissolution or homogeneous dispersion is achieved.
Aqueous Phase Preparation: Prepare 50-100 mL of aqueous solution containing a surfactant (e.g., 1-5% w/v polyvinyl alcohol - PVA) in distilled water. Filter through a 0.45 μm membrane to remove impurities.
Emulsification: Add the organic phase to the aqueous phase dropwise with high-speed homogenization (10,000-15,000 rpm) for 5-10 minutes. Alternatively, use ultrasonication (50-100 W output) for 3-5 minutes with pulse cycles to form a stable o/w emulsion.
Solvent Evaporation: Transfer the emulsion to a round-bottom flask and stir continuously (500-1000 rpm) at room temperature for 4-8 hours or under reduced pressure if using solvents with high boiling points. Monitor the process until complete solvent evaporation is confirmed.
Nanoparticle Recovery: Centrifuge the nanoparticle suspension at 15,000-20,000 × g for 30-60 minutes at 4°C. Wash the pellet 2-3 times with distilled water to remove excess surfactant. Resuspend in appropriate buffer and lyophilize for long-term storage.
Quality Control Parameters:
- Size Analysis: Dynamic light scattering (DLS) to ensure particle size between 80-300 nm
- Polydispersity Index (PDI): <0.3 indicates monodisperse population
- Encapsulation Efficiency: Typically 60-90% depending on drug-polymer compatibility
- Morphology: Spherical morphology confirmed by SEM/TEM
Characterization of PNPs for Cancer Applications
Nuclear Magnetic Resonance (NMR) Spectroscopy:
- Purpose: Monitor polymerisation conversion and kinetics; confirm successful drug-polymer conjugation [31]
- Procedure: Prepare 5-10 mg/mL polymer solution in deuterated solvent (CDCl₃, DMSO-d₆). Acquire ¹H NMR spectra at 25°C. For conjugation confirmation, compare spectra before and after drug loading, noting appearance of new characteristic peaks or chemical shift changes.
- Advanced Applications: Use 2D NMR techniques (COSY, HSQC, HMBC) to investigate local chemical environments near conjugation sites. Apply Diffusion-Ordered Spectroscopy (DOSY) for molecular weight determination.
Dynamic Light Scattering (DLS) and Zeta Potential:
- Purpose: Determine particle size distribution, polydispersity index, and surface charge
- Procedure: Dilute PNP suspension in appropriate buffer (1:100 v/v) to avoid multiple scattering. Measure size at 25°C with detection angle of 90°. For zeta potential, use folded capillary cells and measure electrophoretic mobility, converting to zeta potential using Smoluchowski approximation.
Drug Release Kinetics:
- Purpose: Evaluate drug release profile under physiological and tumor microenvironment conditions
- Procedure: Place 5-10 mg of drug-loaded PNPs in dialysis membrane (MWCO 12-14 kDa) against release medium (PBS, pH 7.4 and acetate buffer, pH 5.5). Maintain at 37°C with constant shaking (100 rpm). Collect samples at predetermined time points (1, 2, 4, 8, 12, 24, 48, 72 hours) and analyze drug content by HPLC/UV-Vis spectroscopy. Replace with fresh medium after each sampling.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for PNP Development in Immunotherapy
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Polymers | PLGA, PCL, PLA, HPMA, Chitosan | Form nanoparticle matrix; control degradation & release kinetics | Molecular weight, block composition, end-group functionality affect properties |
| Targeting Ligands | Folate, Transferrin, RGD peptides, Aptamers, mAbs | Active targeting to cancer cells or immune cells | Conjugation efficiency, orientation, retention of binding affinity post-conjugation |
| Stimuli-Responsive Materials | pH-sensitive (Eudragit), Temperature-sensitive, Enzyme-cleavable linkers | Triggered drug release in tumor microenvironment | Response threshold must match physiological conditions |
| Characterization Standards | Latex beads (size standards), Zeta potential reference | Instrument calibration for accurate measurements | Use appropriate size range matching expected PNP dimensions |
| Therapeutic Payloads | Doxorubicin, Paclitaxel, siRNA, miRNAs, Immune checkpoint inhibitors | Therapeutic effect against cancer | Hydrophobicity/hydrophilicity compatibility with polymer system |
Mechanism of PNP Action in Cancer Immunotherapy
The mechanism of PNP-mediated cancer immunotherapy involves a coordinated sequence of events that enhances antitumor immune responses. As illustrated in the diagram above, functionalized PNPs first navigate through circulation and accumulate in tumor tissue via the EPR effect or active targeting mechanisms [52]. Following cellular internalization, PNPs release their payload (e.g., immunomodulators, antigens, or checkpoint inhibitors) in response to tumor-specific stimuli [12]. These released agents then facilitate dendritic cell maturation and antigen presentation, leading to robust T cell priming and activation [53]. The activated cytotoxic T lymphocytes (CTLs) subsequently recognize and eliminate cancer cells, releasing additional neoantigens that perpetuate the cancer-immunity cycle and establish long-term immunological memory [53]. This comprehensive approach addresses key limitations of conventional immunotherapies by ensuring precise delivery of immunotherapeutic agents to target cells while minimizing systemic exposure and associated adverse events.
Future Perspectives and Challenges
The field of PNP-based cancer immunotherapy continues to evolve with several promising directions. Next-generation systems currently in development include hybrid nanoparticles, stimulus-responsive NPs, and artificial intelligence-directed NPs with programmable and adaptive capabilities for cancer vaccinations and immunotherapy [55]. The integration of AI in optimizing nanoparticle design represents a particularly promising avenue for accelerating development and personalization of PNP-based therapies [12]. However, several challenges must be addressed for clinical translation, including scalability of manufacturing processes, long-term stability of formulations, comprehensive safety assessment, and regulatory compliance [12] [31]. Additionally, understanding the dynamic behavior of PNPs within complex biological systems and their interactions with immune components remains crucial for advancing these promising targeted drug delivery systems toward clinical application [31]. Despite these challenges, the ongoing progress in nano-immunotherapy suggests a promising future where combination nano-immunotherapies will achieve significant success in clinical cancer management.
The blood-brain barrier (BBB) and various ocular barriers represent two of the most formidable challenges in drug delivery for neurological and ophthalmic disorders. The BBB is a highly selective semi-permeable membrane that separates circulating blood from the brain extracellular fluid, with less than 100% of small-molecule drugs and nearly all macromolecular therapeutics unable to cross it effectively [56]. Similarly, ocular barriers—including the cornea, conjunctiva, and blood-retinal barrier—severely restrict drug penetration, resulting in bioavailability of less than 5% for most conventional ophthalmic formulations [57] [58]. These barriers share common protective functions but present distinct structural and physiological challenges that require tailored delivery strategies.
Polymeric nanoparticles (PNPs) have emerged as promising vehicles to overcome these biological barriers. These nanocarriers, typically ranging from 10-1000 nanometers, offer significant advantages including versatile drug encapsulation, controlled release profiles, and surface functionalization capabilities [12] [31]. Their nanoscale dimensions facilitate cellular uptake and navigation of biological barriers, while their polymeric composition enables precise tuning of essential delivery parameters [31]. This application note examines current PNP strategies for enhanced drug delivery across the BBB and ocular barriers, providing structured experimental data and methodologies to support research and development efforts.
Polymeric Nanoparticle Design and Characterization
Material Selection and Formulation Strategies
The rational design of PNPs begins with careful selection of polymer materials, which directly influences nanoparticle physicochemical properties, drug loading capacity, and release kinetics. Both natural and synthetic polymers offer distinct advantages for barrier-specific applications [59].
Natural polymers including chitosan, alginate, hyaluronic acid, and cellulose provide inherent biocompatibility and biodegradability. Chitosan exhibits particularly valuable mucoadhesive properties that prolong residence time in nasal and ocular applications [59]. Synthetic polymers such as poly(lactic-co-glycolic acid) (PLGA), polyethylene glycol (PEG), polylactic acid (PLA), and polyvinyl alcohol (PVA) offer precisely controllable mechanical properties and degradation rates [59]. PLGA is especially widely used due to its established safety profile and tunable erosion kinetics.
Table 1: Common Polymers for Ocular and BBB Drug Delivery
| Polymer Type | Specific Polymer | Key Properties | Primary Applications |
|---|---|---|---|
| Natural | Chitosan | Mucoadhesive, biocompatible, permeation enhancer | Nose-to-brain delivery, ocular surface delivery |
| Natural | Hyaluronic Acid | Bioadhesive, viscoelastic, target for CD44 receptors | Ocular delivery, retinal targeting |
| Natural | Alginate | Ionic crosslinking, mild gelation conditions | Ocular inserts, in situ gelling systems |
| Synthetic | PLGA | Biodegradable, tunable degradation, FDA-approved | Sustained release for both ocular and brain delivery |
| Synthetic | PEG | Stealth properties, reduced protein adsorption | Surface functionalization to improve circulation time |
| Synthetic | PLA | Slower degradation than PLGA, high biocompatibility | Long-term implantable devices, sustained release |
| Synthetic | PVA | Stabilizer, film-forming, high water solubility | Nanoparticle stabilization, ocular inserts |
Advanced formulation strategies include stimuli-responsive systems that release drugs in response to specific physiological triggers such as pH, temperature, or enzyme activity [12] [31]. For instance, pH-sensitive polymers can be designed to release therapeutic payloads in the acidic tumor microenvironment of brain cancers or in inflamed ocular tissues. Additionally, surface functionalization with targeting ligands, cell-penetrating peptides, or mucoadhesive polymers significantly enhances targeting efficiency and cellular uptake [12] [60].
Critical Quality Attributes and Characterization Techniques
Comprehensive characterization of PNPs is essential for predicting in vivo performance and ensuring batch-to-batch consistency. Key physicochemical properties must be carefully controlled and measured using appropriate analytical techniques [31].
Table 2: Key Characterization Parameters for Polymeric Nanoparticles
| Parameter | Target Range | Impact on Performance | Characterization Methods |
|---|---|---|---|
| Particle Size | 50-200 nm for BBB; 100-300 nm for ocular | Cellular uptake, barrier penetration, biodistribution | Dynamic Light Scattering (DLS), Electron Microscopy |
| Polydispersity Index (PDI) | <0.2 | Formulation homogeneity, reproducibility | Dynamic Light Scattering |
| Zeta Potential | ±10-30 mV (context-dependent) | Colloidal stability, mucoadhesion | Electrophoretic Light Scattering |
| Drug Loading Capacity | 5-30% (w/w) | Therapeutic efficacy, dosing frequency | HPLC, UV-Vis Spectroscopy after extraction |
| Encapsulation Efficiency | >80% | Process efficiency, cost-effectiveness | Ultracentrifugation, Gel Permeation Chromatography |
| Release Profile | Variable based on application | Therapeutic kinetics, dosing frequency | Dialysis, Franz Diffusion Cells |
Nuclear Magnetic Resonance (NMR) spectroscopy provides detailed insights into polymer conversion kinetics, successful drug conjugation, and molecular weight determination [31]. Advanced techniques such as Diffusion-ordered NMR (DOSY) can determine molecular weight distributions, while two-dimensional NMR methods (COSY, HSQC, HMBC) offer powerful insights into local chemical environments near conjugation sites [31].
Dynamic Light Scattering remains the gold standard for determining particle size distribution and zeta potential, while electron microscopy (SEM, TEM) provides visual confirmation of nanoparticle morphology and size [31]. Additional characterization should include in vitro drug release studies using dialysis membranes or Franz diffusion cells to establish release kinetics under physiologically relevant conditions.
Overcoming Ocular Barriers
Ocular Anatomy and Delivery Challenges
The eye's complex anatomy presents multiple static and dynamic barriers that effectively limit drug penetration. The anterior segment (cornea, conjunctiva, aqueous humor) is most accessible but still presents significant challenges, with typically less than 5% of topically applied drugs reaching intraocular tissues [57]. The posterior segment (retina, choroid, vitreous humor) is particularly difficult to target, requiring drugs to traverse the blood-retinal barrier or endure invasive administration methods [57].
Common ocular diseases requiring advanced delivery approaches include glaucoma (affecting approximately 80 million people globally), age-related macular degeneration (AMD), diabetic retinopathy, and cataracts [58]. Conventional treatments like eye drops suffer from rapid precorneal clearance (within 15-30 seconds), nasolacrimal drainage, and limited corneal permeability, necessitating frequent administration and resulting in poor patient compliance [57] [58].
PNP Formulations for Ocular Delivery
Various PNP systems have been developed to improve ocular drug delivery, each offering distinct advantages for specific applications:
Polymeric Nanoparticles (e.g., PLGA-based systems) provide sustained drug release and improved corneal penetration. Their small size enables longer residence time in the pre-corneal area and enhanced permeation through corneal epithelium [57]. Nanostructured lipid carriers and solid lipid nanoparticles offer improved biocompatibility and higher drug loading for lipophilic compounds [12]. In situ gelling systems transition from liquid to gel upon contact with the ocular surface, significantly prolonging drug residence time [58].
Experimental studies demonstrate that optimizing nanoparticle size and surface properties is critical for ocular delivery. Particles between 100-300 nm show optimal balance between retention and penetration, with positive surface charge enhancing interaction with negatively charged corneal surfaces [58]. Functionalization with mucoadhesive polymers like chitosan further prolongs residence time by interacting with ocular mucin.
Experimental Protocol: Preparation of PLGA Nanoparticles for Ocular Delivery
Objective: Prepare and characterize pilocarpine-loaded PLGA nanoparticles for sustained glaucoma therapy.
Materials:
- PLGA (50:50 LA:GA ratio, 15 kDa)
- Pilocarpine hydrochloride
- Polyvinyl alcohol (PVA, 30-70 kDa)
- Dichloromethane (DCM)
- Deionized water
- Dialysis membrane (MWCO 12-14 kDa)
Methodology:
- Organic Phase Preparation: Dissolve 100 mg PLGA and 15 mg pilocarpine hydrochloride in 5 mL DCM.
- Aqueous Phase Preparation: Prepare 20 mL of 2% (w/v) PVA solution in deionized water.
- Emulsion Formation: Add the organic phase dropwise to the aqueous phase while probe-sonicating at 70% amplitude for 2 minutes in an ice bath.
- Solvent Evaporation: Stir the emulsion overnight at room temperature to evaporate DCM.
- Nanoparticle Recovery: Centrifuge at 20,000 rpm for 30 minutes at 4°C, wash twice with deionized water, and resuspend in 5 mL deionized water.
- Lyophilization: Add 5% (w/v) trehalose as cryoprotectant and lyophilize for 48 hours.
Characterization:
- Determine particle size, PDI, and zeta potential by DLS
- Assess morphology by TEM
- Calculate drug loading and encapsulation efficiency by HPLC
- Evaluate in vitro release using Franz diffusion cells with simulated tear fluid (pH 7.4)
Overcoming the Blood-Brain Barrier
BBB Structure and Impediments to Drug Delivery
The BBB consists of specialized endothelial cells connected by tight junctions, surrounded by pericytes, astrocytes, and a basement membrane, collectively forming the neurovascular unit [56]. This complex structure expresses various efflux transporters (notably P-glycoprotein) that actively remove foreign compounds, severely restricting drug penetration to the brain [61] [56].
BBB dysfunction is implicated in numerous neurodegenerative diseases. In Alzheimer's disease, compromised BBB integrity is observed with increased permeability, reduction in tight junction proteins, and impaired P-glycoprotein function [61]. Parkinson's disease patients demonstrate albumin infiltration in cerebrospinal fluid and decreased expression of tight junction proteins (ZO-1, occludin, claudin-5) in specific brain regions [61]. These pathological alterations offer both challenges and opportunities for targeted drug delivery.
PNP Strategies for BBB Penetration
PNPs employ multiple mechanisms to overcome the BBB, including receptor-mediated transcytosis, adsorptive-mediated transcytosis, and inhibition of efflux transporters [56]. Surface modification with targeting ligands significantly enhances brain-specific delivery:
Ligand-functionalized PNPs can target receptors highly expressed on BBB endothelial cells, including transferrin receptors, insulin receptors, and low-density lipoprotein receptors [56]. Cell-penetrating peptides (e.g., TAT, penetratin) facilitate cellular uptake through various energy-dependent and independent mechanisms [60]. Stimuli-responsive systems can be designed to release drugs in response to pathological conditions such as elevated enzyme activity or acidic pH in tumor environments [12].
The nose-to-brain delivery approach has gained significant attention as a non-invasive method to bypass the BBB entirely [59] [60]. This route leverages the anatomical connection between the nasal cavity and the brain via olfactory and trigeminal nerve pathways, allowing direct transport of therapeutics to the CNS while minimizing systemic exposure [60].
Experimental Protocol: Nose-to-Brain Delivery of Polymeric Nanoparticles
Objective: Develop and evaluate chitosan-coated PLGA nanoparticles for nose-to-brain delivery of antiepileptic drugs.
Materials:
- PLGA (50:50 LA:GA, 20 kDa)
- Chitosan (medium molecular weight, 85% deacetylated)
- Levetiracetam
- Acetone
- Acetic acid (1% v/v)
- Tripolyphosphate (TPP, 0.1% w/v)
- Fluorescent dye (DiR for in vivo tracking)
Methodology:
- Nanoparticle Preparation: Prepare PLGA nanoparticles loaded with levetiracetam using the nanoprecipitation method.
- Chitosan Coating: Dissolve chitosan in 1% acetic acid solution to obtain 0.5% (w/v) concentration.
- Surface Functionalization: Add PLGA nanoparticles dropwise to chitosan solution under magnetic stirring at 800 rpm for 60 minutes.
- Ionic Crosslinking: Add TPP solution (0.1% w/v) to the nanoparticle suspension and stir for 30 minutes.
- Purification: Centrifuge at 15,000 rpm for 30 minutes and resuspend in phosphate buffer (pH 6.0).
- Characterization: Analyze size, zeta potential, mucoadhesion properties, and in vitro drug release.
In Vivo Evaluation:
- Administer 20 μL of nanoparticle suspension to each nostril of anesthetized rats using a micropipette with soft tubing.
- Sacrifice animals at predetermined time points (0.5, 2, 4, 8, 24 hours).
- Collect brain tissues (olfactory bulb, cortex, cerebellum) and blood samples.
- Analyze drug concentration in tissues using HPLC-MS.
- Perform fluorescence imaging for biodistribution studies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for PNP Formulation and Characterization
| Reagent Category | Specific Examples | Function/Purpose | Application Notes |
|---|---|---|---|
| Polymer Matrix | PLGA (varied LA:GA ratios), PLA, Chitosan, PEG | Structural backbone, determines degradation rate, drug release | PLGA 50:50 most common; molecular weight affects release kinetics |
| Stabilizers/Surfactants | PVA, Poloxamers, Polysorbate 80, D-α-tocopheryl PEG | Prevent aggregation, control particle size, improve stability | PVA (1-3%) most common for emulsion methods; critical for reproducibility |
| Targeting Ligands | Transferrin, Lactoferrin, TAT peptide, RVG29 peptide | Enhance specific cellular uptake, receptor-mediated transcytosis | Conjugation efficiency crucial; must preserve ligand activity |
| Characterization Standards | Latex beads (size standards), Zeta potential reference | Instrument calibration, method validation | Essential for inter-laboratory comparison and data reliability |
| Analytical Tools | HPLC/UPLC systems, DLS, NTA, TEM/SEM | Quantify drug loading, characterize physicochemical properties | Multimethod characterization recommended for comprehensive analysis |
Data Integration and Analysis
The development of PNP formulations for ocular and BBB applications generates complex, multidimensional data. Recent advances in artificial intelligence and machine learning are increasingly employed to identify patterns and optimize formulations more efficiently than traditional trial-and-error approaches [62]. Analysis of existing PLGA nanoparticle datasets reveals several key relationships between formulation parameters and performance metrics:
A strong positive correlation exists between the drug-to-polymer ratio and loading capacity, while a moderate correlation is observed between the PLGA lactide:glycolide (LA:GA) ratio and particle size [62]. These relationships enable more predictive formulation design and reduce development timelines.
Standardized data reporting is essential for advancing the field. Critical data elements include polymer properties (composition, molecular weight, viscosity), formulation parameters (method, solvents, surfactants), physicochemical characteristics (size, PDI, zeta potential), and performance metrics (loading capacity, encapsulation efficiency, release profile) [62]. Shared datasets facilitate community-wide learning and accelerate innovation.
Polymeric nanoparticles represent a versatile and promising platform for overcoming the formidable challenges posed by ocular and blood-brain barriers. Through rational design of particle characteristics, strategic surface functionalization, and appropriate administration routes, PNPs can significantly enhance drug delivery to previously inaccessible therapeutic targets. The continued refinement of formulation methods, characterization techniques, and application-specific designs will further advance the clinical translation of these sophisticated drug delivery systems.
Future development should focus on multifunctional systems that combine targeting, barrier penetration, and controlled release in a single platform. Additionally, advancing our understanding of biological barrier biology in disease states will enable more precise targeting strategies. The integration of computational approaches, including AI and machine learning, will accelerate formulation optimization and facilitate the development of personalized nanomedicines tailored to specific patient populations and disease states.
Polymeric nanoparticles (PNPs) represent a groundbreaking advancement in nanomedicine, offering a versatile platform for encapsulating and delivering a wide spectrum of therapeutic agents [6]. Their nanoscale dimensions (typically 10-1000 nm) facilitate cellular uptake and navigation of biological barriers, including the challenging blood-brain barrier [31]. The core advantage of PNPs lies in their chemical versatility; through various polymerization and functionalization techniques, researchers can create carriers with precisely tailored properties for controlled drug release, enhanced stability, and improved bioavailability while minimizing side effects [6] [31]. This application note details the formulation, characterization, and application protocols for using PNPs to deliver three major therapeutic classes: small molecules, nucleic acids, and natural bioactives, providing a standardized framework for research and development within the broader context of polymeric drug delivery systems.
Polymeric Nanoparticles as Versatile Delivery Vehicles
Polymeric nanoparticles are particularly valuable for addressing the delivery challenges associated with different cargo types. For small molecule drugs, PNPs enhance the solubility and stability of hydrophobic compounds, protecting them from premature degradation and enabling targeted delivery [6] [31]. The encapsulation of small molecules within PNPs like poly(lactic-co-glycolic acid) (PLGA) can significantly improve their pharmacokinetic profiles [63].
For nucleic acid therapeutics—including small interfering RNA (siRNA), microRNA (miRNA), and plasmid DNA (pDNA)—PNPs offer a non-viral delivery vector that protects these large, negatively charged molecules from rapid clearance and nuclease degradation [64]. Cationic polymers can electrostatically condense nucleic acids into polyplexes, facilitating transport into intracellular compartments where they can regulate gene expression [64] [65].
Natural bioactives, such as plant-derived compounds, often face challenges related to poor solubility, low bioavailability, and chemical instability. PNPs provide a protective environment for these compounds, enhancing their therapeutic application potential [6]. The ability to engineer "smart" PNPs that respond to specific physiological stimuli (e.g., pH, temperature, or enzymes) further enables precise drug release in targeted environments, benefiting all three cargo classes [6].
Table 1: Key Advantages of Polymeric Nanoparticles for Different Cargo Types
| Cargo Type | Key Challenges | PNP Solutions | Common Polymer Choices |
|---|---|---|---|
| Small Molecules | Poor solubility, systemic toxicity, rapid clearance | Encapsulation, enhanced bioavailability, controlled release | PLGA, PLA, Chitosan, PEG-PLGA |
| Nucleic Acids | Nuclease degradation, negative charge, unable to cross membranes | Condensation into polyplexes, protection, endosomal escape | PEI, Chitosan, Cationic PLGA |
| Natural Bioactives | Chemical instability, poor bioavailability, first-pass metabolism | Stabilization, protection from degradation, improved absorption | PLGA, Chitosan, Gantrez AN-119 |
Experimental Protocols for PNP Formulation and Characterization
Microfluidic Nanoprecipitation for PNP Formulation
Microfluidic nanoprecipitation enables superior control over nanoparticle size and polydispersity compared to traditional batch methods [63]. The following protocol is optimized for PLGA-based nanoparticles.
Materials:
- Polymer: PLGA (Resomer RG 502 H, Mw 7000–17,000 Da)
- Organic Solvent: Acetonitrile (ACN, 99.95%)
- Aqueous Phase: Polyvinyl alcohol (PVA, 9000–10,000 Mw, 80% hydrolyzed) solution
- Equipment: Commercial microfluidic platform (e.g., Tamara, Inside Therapeutics) with herringbone mixer chips
Procedure:
- Preparation of Solutions: Dissolve PLGA in ACN at a concentration of 10-30 mg/mL to form the organic phase. Prepare an aqueous PVA solution (1.5-2.5% w/v) as the antisolvent phase.
- Microfluidic Setup: Prime the microfluidic system according to manufacturer instructions. Use a chip with a three-inlet junction geometry for superior mixing efficiency.
- Optimized Flow Parameters: Set the Flow Rate Ratio (FRR - aqueous-to-organic) to 3:1 and Total Flow Rate (TFR) to 12 mL/min. These parameters produce smaller, more uniform nanoparticles (~130 nm) with low PDI (~0.1) [63].
- Collection and Purification: Collect the nanoparticle suspension and incubate overnight to allow for complete solvent evaporation. Centrifuge at 15,000 rpm for 20 minutes, wash twice with deionized water, and lyophilize for long-term storage.
Batch Method Alternative: For traditional batch nanoprecipitation, add the organic phase dropwise to the aqueous phase under continuous magnetic stirring at 660 rpm. While more accessible, this method typically yields larger particles with broader size distribution (PDI > 0.2) [63].
Comprehensive Characterization of PNPs
Rigorous characterization is essential to correlate PNP properties with biological performance [31].
Size and Morphology Analysis:
- Dynamic Light Scattering (DLS): Measure hydrodynamic diameter and polydispersity index (PDI). Dilute samples in buffer to avoid scattering saturation.
- Electron Microscopy: Use Transmission Electron Microscopy (TEM) or cryo-TEM for direct visualization of nanoparticle size, morphology, and internal structure [66] [31].
Surface Charge and Chemistry:
- Zeta Potential: Measure using electrophoretic light scattering in diluted suspension. Values > ±30 mV indicate good colloidal stability.
- Nuclear Magnetic Resonance (NMR) Spectroscopy: Employ diffusion-ordered (DOSY) NMR to determine molecular weight and confirm successful drug-polymer conjugation [31].
Drug Loading and Release:
- Encapsulation Efficiency: Determine by quantifying free drug in supernatant after centrifugation using HPLC or UV-Vis spectroscopy.
- In Vitro Release Studies: Use Franz diffusion cells or dialysis membranes in appropriate buffer (e.g., PBS, pH 7.4). Sample at predetermined intervals and analyze drug content.
Table 2: Essential Characterization Techniques for Polymeric Nanoparticles
| Property | Characterization Technique | Key Information Obtained | Ideal Range for Drug Delivery |
|---|---|---|---|
| Size & Distribution | Dynamic Light Scattering (DLS) | Hydrodynamic diameter, PDI | 50-200 nm for enhanced permeability and retention |
| Surface Charge | Zeta Potential Measurement | Surface charge, colloidal stability | > ±30 mV for stable formulations |
| Morphology | Transmission Electron Microscopy (TEM) | Particle shape, core-shell structure | Spherical, uniform morphology |
| Chemical Structure | Nuclear Magnetic Resonance (NMR) | Polymer composition, drug conjugation | Confirmation of successful conjugation |
| Crystallinity | X-ray Diffraction (XRD) | Physical state of encapsulated drug | Amorphous dispersion for enhanced solubility |
| Surface Composition | X-ray Photoelectron Spectroscopy (XPS) | Elemental composition, surface chemistry | Verification of surface functionalization |
Nucleic Acid Complexation and Transfection Protocol
For nucleic acid delivery, polyplex formation relies on electrostatic interactions between cationic polymers and anionic nucleic acids [64].
Polyplex Formation:
- N/P Ratio Calculation: Calculate the required N/P ratio (number of polymer nitrogen atoms per nucleic acid phosphate). Begin with N/P ratios of 5-20 for optimal complexation.
- Complexation Procedure: Dilute cationic polymer (e.g., PEI, chitosan) and nucleic acid in separate vials using appropriate buffer. Slowly add the polymer solution to the nucleic acid solution with gentle vortexing.
- Incubation: Incubate the mixture at room temperature for 30 minutes to allow polyplex formation.
Characterization and Transfection:
- Gel Retardation Assay: Analyze polyplex formation by agarose gel electrophoresis to confirm complete nucleic acid complexation.
- Size and Zeta Potential: Measure polyplex hydrodynamic diameter and surface charge as described in section 3.2.
- In Vitro Transfection: Seed cells in 24-well plates 24 hours prior to transfection. Add polyplexes equivalent to 0.1-1 μg nucleic acid per well. Analyze gene expression after 24-72 hours.
Advanced Formulation Strategies and Scale-Up
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Polymeric Nanoparticle Research
| Reagent/Material | Function/Application | Examples/Notes |
|---|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | Biodegradable polymer backbone for nanoparticle matrix | Resomer series (Evonik); varying lactic:glycolic ratios control degradation rate |
| PVA (Polyvinyl Alcohol) | Stabilizer/surfactant in nanoprecipitation | 9000-10,000 Mw, 80% hydrolyzed; concentration affects particle size and PDI |
| Cationic Polymers (PEI, Chitosan) | Nucleic acid complexation and condensation | Branched PEI (25 kDa) for high transfection; chitosan for improved biocompatibility |
| PEG Derivatives | Surface functionalization for stealth properties | PEG-PLGA diblock copolymers reduce opsonization and extend circulation half-life |
| Targeting Ligands | Active targeting to specific cells/tissues | Folate, peptides, antibodies, or aptamers conjugated to nanoparticle surface |
| Fluorescent Dyes | Tracking and biodistribution studies | Cyanine dyes (Cy5, Cy7), FITC, or Rhodamine for in vitro and in vivo imaging |
Computational Fluid Dynamics for Process Optimization
Computational Fluid Dynamics (CFD) modeling provides insights into mixing efficiency within microfluidic devices. Simulations reveal that a three-inlet junction design creates significantly more homogeneous mixing and efficient interfacial contact compared to standard Y-junction designs, resulting in smaller, more uniform nanoparticles [63]. This integrated approach of experimental optimization with numerical modeling provides a robust framework for rational design of scalable nanomedicine production systems.
Addressing the Translational Gap
Despite promising preclinical results, fewer than 0.1% of published nanomedicines achieve clinical approval [8]. This translational gap stems from over-reliance on the Enhanced Permeability and Retention (EPR) effect, which is highly heterogeneous in human tumors compared to robust animal models [8]. Successful translation requires:
- Advanced Formulation Strategies: Focus on integrated approaches beyond nanoparticle design alone, considering final dosage forms (sterile injectables, hydrogels, dry powder inhalers) [8].
- Scalable Manufacturing: Implement Quality by Design (QbD) principles and microfluidic technologies to ensure batch-to-batch consistency [63].
- Overcoming Biological Barriers: Develop active targeting strategies and stimuli-responsive systems to move beyond passive EPR reliance [6] [8].
Polymeric nanoparticles provide a highly adaptable platform for delivering diverse therapeutic cargo, from small molecules to nucleic acids and natural bioactives. The protocols outlined in this application note provide researchers with standardized methods for PNP formulation, characterization, and application. As the field advances, the integration of computational modeling, scalable manufacturing, and targeted delivery strategies will be crucial for bridging the translational gap and realizing the full clinical potential of polymeric nanomedicines. Future research should focus on developing robust, biocompatible systems with enhanced target specificity to address previously "undruggable" targets and improve patient outcomes across a wide range of diseases.
Overcoming Hurdles: Tackling Toxicity, Stability, and Scalability Challenges
For polymeric nanoparticles (PNPs) to function effectively as targeted drug delivery systems, they must navigate the complex environment of the bloodstream and evade the body's innate immune surveillance. Upon intravenous administration, nanoparticles are immediately recognized by the immune system, primarily the mononuclear phagocyte system (MPS), leading to rapid clearance from the bloodstream and significantly reduced therapeutic efficacy. [67] The strategic engineering of nanoparticle surfaces to minimize these non-specific interactions is therefore a cornerstone of modern nanomedicine. This "stealth" effect is critical for prolonging systemic circulation time, increasing the likelihood of nanoparticle accumulation at the target site, and improving overall therapeutic outcomes. [12] [68] [67] For decades, poly(ethylene glycol) (PEG) has been the gold-standard polymer for conferring stealth properties. However, growing awareness of its limitations, particularly its immunogenicity, has spurred the development of a new generation of alternative materials and strategies. [69] [70] [67] This application note details the mechanisms, protocols, and emerging alternatives in the field of stealth nanotechnology for drug delivery professionals.
PEGylation: Mechanisms, Protocols, and Limitations
Mechanism of Action of PEG Stealth Properties
PEGylation—the covalent attachment or physical incorporation of PEG chains onto nanoparticle surfaces—confers stealth through two primary mechanisms. First, the hydrophilic PEG chains form a dense, flexible brush-like corona that creates a steric hydration layer. This layer physically hinders the adsorption of opsonin proteins, which are blood serum proteins that tag foreign particles for immune clearance. [71] [72] Second, this steric barrier reduces nonspecific interactions with immune cells, such as macrophages, thereby minimizing phagocytosis and prolonging the nanoparticle's circulation half-life. [68] [67] The effectiveness of this stealth coating is highly dependent on PEG's molecular weight, chain density, and conformation (e.g., "mushroom" vs. "brush" regimes). [67]
Standard Protocol: PEGylation of PLGA Nanoparticles via Emulsion-Solvent Evaporation
The following protocol describes a standard method for preparing PEGylated PLGA nanoparticles, a widely used biodegradable system. [72]
Objective: To fabricate drug-loaded, PEGylated PLGA nanoparticles with a controlled size distribution and a stealth PEG corona.
Materials:
- Polymers: PLGA (e.g., 50:50 LA:GA, MW 40,000 Da), mPEG-PLGA block copolymer (PEG MW 2000-5000 Da).
- Drug: Active Pharmaceutical Ingredient (API) of interest (e.g., Doxorubicin).
- Solvents: Dichloromethane (DCM), high purity.
- Aqueous Phase: Polyvinyl Alcohol (PVA) solution (1-2% w/v in Milli-Q water).
- Equipment: Probe sonicator, magnetic stirrer/hot plate, vacuum evaporator, centrifugation system, dynamic light scattering (DLS) instrument, Zeta potential analyzer.
Procedure:
- Organic Phase Preparation: Dissolve 100 mg of PLGA and 10-20 mg of mPEG-PLGA copolymer along with 5-10 mg of the drug in 5 mL of DCM. Stir until the polymers are completely dissolved.
- Emulsification: Add the organic phase dropwise to 50 mL of 1% PVA solution under continuous probe sonication (e.g., 100 W, 2 minutes on ice) to form a stable oil-in-water (o/w) emulsion.
- Solvent Evaporation: Transfer the emulsion to a beaker and stir magnetically at room temperature for 4-6 hours to allow the DCM to evaporate fully, solidifying the nanoparticles.
- Purification: Centrifuge the nanoparticle suspension at 20,000 rpm for 30 minutes at 4°C. Discard the supernatant and resuspend the pellet in Milli-Q water. Repeat this washing step three times to remove excess PVA and unencapsulated drug.
- Characterization:
- Size and PDI: Dilute a sample of the nanoparticle suspension and analyze using DLS to determine the hydrodynamic diameter and polydispersity index (PDI). Target size is typically 100-200 nm with a PDI <0.2.
- Zeta Potential: Measure the surface charge of the nanoparticles in a neutral buffer. Successful PEGylation often results in a zeta potential near neutral (e.g., -5 to +5 mV).
- Drug Loading & Encapsulation Efficiency: Lyophilize a known amount of purified nanoparticles. Dissolve them in DCM or a suitable solvent and quantify the drug content using HPLC or UV-Vis spectroscopy to calculate loading capacity and encapsulation efficiency. [72]
The PEG Dilemma: Immunogenicity and Limitations
Despite its widespread use, PEGylation faces significant challenges. The "PEG dilemma" refers to the trade-off where the steric barrier that prolongs circulation also inhibits desired interactions, such as cellular uptake and endosomal escape, potentially reducing therapeutic efficacy. [71] More critically, PEG can be immunogenic. Repeated administration can trigger the production of anti-PEG antibodies (Abs), leading to the Accelerated Blood Clearance (ABC) phenomenon, where subsequent doses are cleared rapidly from the bloodstream, and potentially to severe hypersensitivity reactions. [70] [71] [67] Pre-existing anti-PEG antibodies have been found in a significant portion of the treatment-naïve population, linked to the widespread use of PEG in cosmetics and pharmaceuticals. [70]
Diagram 1: The PEG Immunogenicity Problem. Initial exposure to PEGylated nanoparticles can trigger anti-PEG antibody production, leading to Accelerated Blood Clearance (ABC) and reduced efficacy upon repeated dosing. [70] [71]
Beyond PEG: Emerging Strategies and Alternatives
The limitations of PEG have catalyzed the search for next-generation stealth materials. The ideal alternative should combine low immunogenicity with effective stealth properties and not hinder cellular uptake.
Table 1: Quantitative Comparison of PEG and Leading Alternative Stealth Polymers
| Polymer / Strategy | Key Mechanism & Structure | Reported Advantages over PEG (Preclinical) | Potential Challenges |
|---|---|---|---|
| Linear PEG [71] [67] | Hydrophilic polymer forming a hydrated steric barrier. | Gold standard, well-characterized, long circulation half-life. | Immunogenicity, ABC phenomenon, steric hindrance. |
| Poly(carboxybetaine) (PCB) [69] [71] | Zwitterionic polymer; creates a strong hydration shell via electrostatic interactions. | Superior reduction in protein adsorption; enhances endosomal escape via membrane interactions; low immunogenicity in repeated dosing. | Synthetic complexity; long-term in vivo fate requires further study. |
| Brush-Shaped Polymers (BPLs) [69] [71] | High-density brush architecture with short PEG side chains. | Reduces binding of anti-PEG antibodies; maintains prolonged circulation; compatible with repeated dosing. | Optimization of structure (side-chain length, DP) is complex. |
| Hydroxyl-PEG (HO-PEG) [71] | PEG lipid with a terminal hydroxyl group instead of methoxy. | Demonstrated lower immunogenicity; validated in clinical-stage formulations (e.g., Moderna). | Still a PEG derivative, potential for residual immunogenicity. |
Protocol: Formulating mRNA-LNPs with PCB-Lipids as a PEG Alternative
This protocol is adapted from recent studies on zwitterionic polymer lipids for mRNA delivery. [69] [71]
Objective: To prepare and characterize mRNA-loaded lipid nanoparticles (LNPs) using poly(carboxybetaine) (PCB)-lipids as a stealth stabilizer instead of conventional PEG-lipids.
Materials:
- Lipids: Ionizable cationic lipid (e.g., SM-102), DSPC, Cholesterol, PCB-lipid (e.g., PCB-DMG).
- Aqueous Phase: mRNA in citrate buffer (pH 4.0).
- Organic Phase: Ethanol.
- Equipment: Microfluidic mixer (e.g., NanoAssemblr), PD-10 desalting columns, DLS instrument, fluorescence spectrophotometer.
Procedure:
- Lipid Stock Solution: Prepare the lipid mixture by dissolving the ionizable lipid, DSPC, cholesterol, and PCB-lipid at a defined molar ratio (e.g., 50:10:38.5:1.5) in ethanol.
- Microfluidic Mixing: Load the lipid ethanolic solution and the mRNA aqueous solution into separate syringes. Pump both streams at a fixed flow rate (e.g., 1:3 volumetric ratio) into a microfluidic chip to facilitate rapid mixing and LNP self-assembly.
- Buffer Exchange: After collection, dialyze the formed LNPs against PBS (pH 7.4) or use a desalting column to remove residual ethanol and exchange the buffer.
- Characterization and Analysis:
- Physicochemical Properties: Use DLS to measure particle size, PDI, and zeta potential.
- mRNA Encapsulation Efficiency: Quantify using a Ribogreen assay. Compare fluorescence values of intact LNPs (with Triton X-100) vs. free mRNA in supernatant to calculate the percentage of encapsulated mRNA.
- In Vitro Transfection: Treat cells (e.g., HEK293, HeLa) with PCB-LNPs and PEG-LNPs containing reporter mRNA (e.g., GFP or Luciferase). Measure protein expression after 24-48 hours using flow cytometry or luminescence assays. PCB-LNPs have demonstrated significantly higher transfection efficiency. [71]
- Anti-PEG Antibody Binding Assay: Incubate LNPs with serum containing anti-PEG antibodies. Analyze by ELISA or DLS to monitor aggregation; PCB-LNPs should show minimal binding and aggregation compared to PEG-LNPs. [69] [71]
Diagram 2: Workflow for Evaluating PEG-Alternative LNPs. The process involves fabricating LNPs with alternative stealth polymers (e.g., PCB) and rigorously testing their performance and immunogenicity in repeated dosing regimens. [69] [71]
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Research Reagent Solutions for Stealth Nanoparticle Development
| Category | Item / Reagent | Function / Application | Example & Notes |
|---|---|---|---|
| Polymers | mPEG-PLGA | Forms stealth corona on biodegradable PNPs; controls drug release kinetics. | Widely used copolymer for sustained release formulations. [72] |
| DMG-PEG2000 | Standard PEG-lipid for stabilizing LNPs; provides initial stealth properties. | Component of early commercial mRNA vaccines; benchmark for new studies. [71] | |
| PEG Alternatives | PCB-Lipids | Zwitterionic PEG alternative; enhances endosomal escape and reduces immunogenicity. | Demonstrated higher mRNA transfection efficiency and compatibility with repeated dosing. [69] [71] |
| Brush Polymer Lipids (BPLs) | High-density brush-shaped PEG derivative; reduces anti-PEG antibody binding. | Engineered to adopt "mushroom" regime, evading immune recognition. [71] | |
| HO-PEG Lipids | PEG-lipid with hydroxyl terminus; lower immunogenicity profile. | Used in Moderna's clinical-stage therapies (e.g., OL-56 lipid). [71] | |
| Characterization Kits | Ribogreen Assay Kit | Quantifies mRNA encapsulation efficiency in LNPs. | Critical for evaluating the quality of nucleic acid-loaded nanoparticles. |
| Dynamic Light Scattering (DLS) | Measures hydrodynamic diameter, PDI, and stability of nanoparticles. | Standard technique for nanomedicine quality control. [31] [72] | |
| Analytical Tools | Anti-PEG ELISA Kit | Detects and quantifies anti-PEG antibodies in serum samples. | Essential for assessing the immunogenicity risk of formulations. [70] |
Ensuring Biocompatibility and Controlled Biodegradation
The efficacy and safety of polymeric nanoparticle (PNP)-based drug delivery systems are fundamentally governed by two interrelated properties: biocompatibility and controlled biodegradation. For researchers and drug development professionals, mastering these properties is critical for translating laboratory innovations into clinically viable therapies. Biocompatibility ensures that the nanoparticle system, its degradation products, and its metabolic by-products do not elicit adverse immune responses or cytotoxic effects [12] [73]. Concurrently, controlled biodegradation dictates the release kinetics of the therapeutic payload and ensures the carrier is safely cleared from the body, preventing long-term accumulation [26] [74]. Within the broader thesis of PNP drug delivery, this document provides detailed application notes and experimental protocols to systematically evaluate and ensure these vital characteristics, forming the foundation for clinically translatable nanomedicines.
Background and Significance
The design of modern PNPs has evolved from simple inert carriers to sophisticated "smart" systems that respond to specific physiological stimuli. A primary advantage of polymeric systems is their versatility; using biodegradable polymers such as poly(lactic-co-glycolic acid) (PLGA), poly(lactic acid) (PLA), and chitosan allows researchers to engineer degradation profiles that match therapeutic timelines [17] [11]. The degradation rate of the polymer matrix is a primary driver of drug release kinetics, enabling sustained release that can maintain therapeutic drug levels for extended periods, thereby reducing dosing frequency and minimizing side effects [75] [12].
Furthermore, the biodegradation process can be tailored to be responsive to the pathological microenvironment. For instance, the accumulation of hydrogen peroxide (H₂O₂) at sites of inflammation or oxidative stress provides a unique trigger for targeted drug release. Advanced polymeric capsules have been developed that undergo backbone degradation upon exposure to biologically relevant concentrations of H₂O₂ (50-100 µM), enabling precise drug delivery to diseased tissue while remaining stable in healthy tissue [74]. This level of control, integral to the rational design of PNPs for delivering sensitive biologics, underscores the need for robust and standardized testing protocols to characterize these systems accurately [26] [9].
The following tables consolidate key quantitative findings from recent research on the relationship between nanoparticle composition, biological properties, and degradation triggers.
Table 1: Biocompatibility and Antibacterial Properties of 3D Printed PLA-ZnO Nanocomposites [76]
| Filler Loading (wt%) | Filler Treatment | Cytotoxicity (against THP-1 cells) | Antibacterial Efficacy (% Reduction) | Suitability for Clinical Use |
|---|---|---|---|---|
| < 2% | Untreated or Silane-treated | Non-cytotoxic after 7 days | >99% (vs. S. aureus & E. coli) | Excellent candidate |
| 2% - 5% | Untreated or Silane-treated | Non-cytotoxic after 7 days | >99% (vs. S. aureus & E. coli) | Potential candidate |
| 5% | Untreated or Silane-treated | Cytotoxic effects evident | >99% (vs. S. aureus & E. coli) | Not appropriate |
Table 2: Degradation Kinetics and Cargo Release of H₂O₂-Sensitive Polymeric Nanoparticles [74]
| Polymer Structure | Linkage Type | H₂O₂ Concentration | Time for 50% Dye Release | Sensitivity to Biologically Relevant H₂O₂ |
|---|---|---|---|---|
| Polymer 1 | Direct linkage | 1 mM | 26 hours | No |
| Polymer 2 | Ether linkage | 1 mM | ~10 hours | Yes |
| Polymer 2 | Ether linkage | 100 µM | ~10 hours | Yes (50-100 µM range) |
Experimental Protocols
Protocol: Assessing H₂O₂-Triggered Degradation and Release Kinetics
This methodology details the evaluation of oxidative stress-responsive PNPs, a key technology for targeted delivery to inflamed tissues [74].
I. Materials and Equipment
- Polymers: H₂O₂-sensitive polymer (e.g., Polymer 2 with ether linkage).
- Model Drug: Nile red or similar solvatochromic dye.
- Formulation Equipment: Probe sonicator, magnetic stirrer.
- Characterization Instruments: Dynamic Light Scattering (DLS) for size and zeta potential, Scanning Electron Microscope (SEM) for morphology.
- Release Study Equipment: Fluorescence spectrophotometer, phosphate-buffered saline (PBS, pH 7.4), hydrogen peroxide solutions (e.g., 100 µM, 1 mM in PBS).
II. Step-by-Step Procedure
- Nanoparticle Formulation: Prepare Nile red-loaded nanoparticles using an oil/water single emulsion-solvent evaporation technique.
- Dissolve 50 mg of H₂O₂-sensitive polymer and 500 µg of Nile red in 2 mL of a suitable organic solvent (e.g., dichloromethane).
- Emulsify this organic phase in 10 mL of a 1% (w/v) polyvinyl alcohol (PVA) aqueous solution using probe sonication on ice for 2-3 minutes.
- Stir this emulsion magnetically overnight at room temperature to allow for solvent evaporation and nanoparticle hardening.
- Collect the nanoparticles by ultracentrifugation (e.g., 20,000 rpm for 30 minutes) and wash three times with distilled water to remove residual PVA and unencapsulated dye.
- Nanoparticle Characterization:
- Size and Zeta Potential: Re-disperse a pellet aliquot in purified water and analyze using DLS.
- Morphology: Examine the nanoparticle morphology using SEM.
- Encapsulation Efficiency (EE): Determine EE by dissolving a known amount of nanoparticles in DMSO and measuring Nile red fluorescence against a standard curve. Calculate EE% = (Mass of drug in nanoparticles / Total mass of drug used) × 100.
- H₂O₂-Triggered Release Study:
- Divide the Nile red-loaded nanoparticle suspension into several aliquots.
- Incubate these aliquots with different concentrations of H₂O₂ (0 µM as control, 50 µM, 100 µM, 1 mM) in PBS at 37°C under gentle agitation.
- At predetermined time intervals, centrifuge samples to separate nanoparticles from the release medium.
- Measure the fluorescence of the supernatant (excitation/emission ~552/636 nm for Nile red). The quenching of fluorescence upon release into the aqueous medium indicates payload release.
- Plot the cumulative release percentage versus time to determine degradation and release kinetics.
III. Data Analysis and Interpretation
- Compare release profiles across different H₂O₂ concentrations. A successful, sensitive formulation will show significantly faster release in the presence of biologically relevant H₂O₂ concentrations (50-100 µM) compared to the control [74].
- Kinetics data can be fitted to various mathematical models (e.g., zero-order, first-order, Higuchi) to understand the underlying release mechanism.
Protocol: Cytotoxicity and Biocompatibility Assessment
This protocol provides a standardized method for evaluating the safety profile of PNPs and their components, such as polymer matrices and functional fillers [76].
I. Materials and Equipment
- Cell Line: Human immune THP-1 cells or other relevant cell lines (e.g., HeLa, HEK293).
- Culture Materials: Cell culture medium (e.g., RPMI-1640), fetal bovine serum (FBS), penicillin-streptomycin, trypsin-EDTA.
- Test Materials: PNP suspensions at various concentrations, pristine polymer solutions, filler particles (e.g., ZnO).
- Assay Kits: MTT or MTS cell viability assay kit.
- Equipment: CO₂ incubator, biological safety cabinet, cell culture plates (96-well), microplate reader.
II. Step-by-Step Procedure
- Cell Seeding:
- Culture THP-1 cells in complete medium at 37°C in a 5% CO₂ atmosphere.
- Seed cells into 96-well plates at a density of 1 x 10⁴ cells per well in 100 µL of medium.
- Incubate for 24 hours to allow cell attachment.
- Treatment with Test Materials:
- Prepare a dilution series of the test articles (PNPs, polymer, filler) in culture medium. Ensure a wide concentration range is tested (e.g., corresponding to filler loadings from 0.5 wt% to 5 wt% for composites).
- Aspirate the medium from the 96-well plate and replace it with 100 µL of the treatment medium containing the test articles. Include wells with medium only (blank) and cells with medium only (untreated control).
- Incubate the plates for the desired exposure period (e.g., 24, 48, and 72 hours).
- Cell Viability Assessment (MTT Assay):
- After the exposure period, carefully add 10 µL of MTT reagent (5 mg/mL in PBS) to each well.
- Incubate the plate for 2-4 hours at 37°C.
- Carefully remove the medium and dissolve the formed formazan crystals in 100 µL of an organic solvent like DMSO.
- Measure the absorbance of each well at 570 nm using a microplate reader.
- Data Analysis:
- Calculate the percentage of cell viability relative to the untreated control: Viability (%) = (Absorbance{treated} - Absorbance{blank}) / (Absorbance{control} - Absorbance{blank}) × 100.
- Plot cell viability against the concentration of the test material to determine the IC₅₀ or the maximum safe concentration.
III. Data Interpretation
- A material is generally considered non-cytotoxic if cell viability remains above 70-80% after exposure, according to international standards like ISO 10993-5 [76].
- As demonstrated in Table 1, note that cytotoxicity is often concentration-dependent, and an optimal "window" of safety and efficacy must be identified [76].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents for Biocompatibility and Degradation Studies
| Reagent/Material | Function and Rationale | Example Applications |
|---|---|---|
| PLA & PLGA | Biodegradable, FDA-approved polymers that hydrolyze into metabolizable lactic and glycolic acids; backbone of many PNP systems. | Core matrix for sustained-release nanoparticles [11]. |
| H₂O₂-Sensitive Polymers (e.g., with ether-linked boronic esters) | Enable targeted drug release in microenvironments with elevated oxidative stress (e.g., inflammation, tumors). | Stimuli-responsive carriers for site-specific delivery [74]. |
| Zinc Oxide (ZnO) Nanofillers | Impart antibacterial functionality; their release rate from a polymer matrix governs biological activity and cytotoxicity. | Antibacterial composites for medical devices [76]. |
| Polyvinyl Alcohol (PVA) | Acts as a surfactant and stabilizer during nanoemulsion formulation, preventing nanoparticle aggregation. | Stabilizing agent in single emulsion methods [11]. |
| Solvatochromic Dye (Nile Red) | Model hydrophobic drug; fluorescence is quenched in aqueous environments, allowing real-time monitoring of release. | Probe for tracking degradation and release kinetics [74]. |
| THP-1 Cell Line | Human monocytic cell line; model for assessing immune cell cytotoxicity and biocompatibility. | In vitro safety profiling of nanoparticles [76]. |
Schematic of Oxidative Degradation Mechanism
The mechanism of H₂O₂-triggered polymer degradation involves a specific chemical cascade that leads to backbone cleavage.
The translation of polymeric nanoparticle (PNP) drug delivery systems from promising laboratory prototypes to commercially viable, clinically effective medicines represents a critical bottleneck in nanomedicine. While PNPs offer significant advantages—including enhanced drug solubility, improved therapeutic index, and targeted delivery capabilities—their clinical translation often remains hampered by uncontrolled and poorly scalable production processes [5] [77]. The inherent properties of nanomedicines, determined by their size, surface characteristics, drug loading, and targeting potential, must be meticulously preserved during scale-up, requiring high reproducibility, homogeneity, and stringent control over nanoparticle properties [5]. Conventional small-scale laboratory synthesis techniques for PNPs are frequently subject to problematic batch-to-batch variability, and increasing the installation size from laboratory scale to industrial scale presents substantial engineering and biological challenges [5] [78]. This Application Note systematically addresses these scale-up hurdles, providing structured data, detailed protocols, and visualization tools to guide researchers and drug development professionals in bridging this critical gap.
Key Scale-Up Challenges and Comparative Analysis
Scaling up PNP production introduces multiple interrelated challenges that extend beyond simple volume increase. The core difficulties stem from maintaining critical quality attributes (CQAs) while transitioning from low-volume, manually-controlled processes to high-volume, automated systems. Table 1 summarizes the primary scale-up challenges and their potential mitigation strategies.
Table 1: Key Scale-Up Challenges and Mitigation Strategies for Polymeric Nanoparticles
| Challenge Category | Specific Scale-Up Hurdles | Potential Mitigation Strategies |
|---|---|---|
| Process Reproducibility | Batch-to-batch variability; Inconsistent mixing dynamics; Particle growth control difficulties [5] [78] | Implement continuous manufacturing; Automated process control; Advanced mixing technologies (e.g., CJM, microfluidics) [77] |
| Product Quality Control | Maintaining size distribution (PDI); Drug loading efficiency; Surface characteristics [8] | Real-time monitoring; Process Analytical Technologies (PAT); Quality by Design (QbD) approaches [8] |
| Manufacturing Feasibility | Organic solvent removal; Residual solvent control; High production costs [78] | Switch to less toxic solvents (e.g., ethyl acetate); Supercritical fluid technology; Membrane-based purification [54] [78] |
| Technical Limitations | Poor solvent power of alternative systems; Energy-intensive processes; Metal contamination risk [78] | Hybrid technologies; Material-specific method selection; Closed-system processing [78] |
| Biological Performance | Weak correlation between in vitro attributes and in vivo performance [8] | Develop improved predictive models; Standardized CQA metrics [8] |
The complexity of these challenges necessitates a systematic approach to process optimization and technology selection. Different production methods offer distinct advantages and limitations for scale-up, as detailed in Table 2.
Table 2: Scale-Up Feasibility of Polymeric Nanoparticle Production Methods
| Production Method | Key Advantages for Scale-Up | Scale-Up Limitations | Particle Size Range |
|---|---|---|---|
| Nanoprecipitation | Small particle size; Low cost; Simplicity [78] | Difficulties controlling particle growth; Applicable mainly to lipophilic drugs [78] | 50-500 nm [54] |
| Microfluidizer Technology | Precise size control; Scalable process; Continuous operation [78] | Multiple cycles required (50-100); High pressure operation [78] | 50-500 nm [78] |
| Supercritical Fluid Technology | Narrow size distribution; Mild temperatures; No residual solvent [78] | Poor solvent power of CO₂; High cost; Voluminous CO₂ usage [78] | 100-1000 nm [78] |
| Solvent Evaporation | Well-established; High efficiency [54] | Organic solvent residues; Batch-to-batch variability [54] | 80-900 nm [54] |
| Automated Coaxial Jet Mixing (CJM) | Stable continuous operation (up to 24h); Tunable size; User-independent [77] | Limited to specific polymer-solvent systems; Initial setup complexity [77] | 56-79 nm (demonstrated) [77] |
Experimental Protocols for Scale-Up Production
Automated Coaxial Jet Mixing (CJM) for Continuous Production
The automated CJM system enables stable, tunable, and continuous production of polymeric NPs, which is essential for scale-up and translation [77]. This protocol describes the setup and operation for continuous production of PEG--b-PLA nanoparticles.
Materials and Equipment:
- Block copolymers: PEG₅K--b-PLA₂₀K, PEG₅K--b-PLGA₂₀K, or PEG₅K--b-PCL₂₀K [77]
- Solvents: Acetonitrile (ACN) for PEG--b-PLA and PEG--b-PCL; Dimethylformamide (DMF) for PEG--b-PLGA [77]
- Aqueous phase: Ultrapure deionized water (dH₂O), freshly filtered using 0.22 μm membrane
- Equipment: Computer-controlled syringe pumps, CJM assembly from off-the-shelf components (detailed in Bovone et al., 2019 [77])
Procedure:
Polymer Solution Preparation: Prepare block copolymer solution at 10 mg/mL or 50 mg/mL in appropriate solvent (ACN for PEG--b-PLA/PCL; DMF for PEG--b-PLGA). Filter through 0.22 μm membrane.
System Setup and Priming:
- Assemble CJM according to manufacturer specifications
- Connect organic phase (polymer solution) and aqueous phase (dH₂O) to separate syringe pumps
- Prime both lines to remove air bubbles
- Initialize computer control system for flow rate regulation
Process Optimization and Operation:
- Set initial flow rate ratio (aqueous:organic) to 10:1
- Systematically vary total flow rate (1-10 mL/min) and flow rate ratio to tune nanoparticle size
- Collect nanoparticle suspension in clean receptacle
- Operate system continuously for target duration (up to 24 hours demonstrated)
Post-Processing:
- Remove organic solvent by reduced pressure evaporation or dialysis
- Concentrate nanoparticles using tangential flow filtration if needed
- Sterilize by 0.22 μm filtration for biomedical applications
Critical Parameters:
- Flow rate ratio: Primary determinant of nanoparticle size [77]
- Polymer concentration: Affects size and polydispersity
- Total flow rate: Influences mixing efficiency and particle characteristics
- Polymer chemistry: Requires tuning of flow conditions for different block copolymers [77]
Microfluidizer Technology for Scalable Production
Microfluidizer technology utilizes high-pressure homogenization to produce nanoparticles with precise size control, offering scalability for industrial production [78].
Materials and Equipment:
- Polymers: PLGA, PCL, or other biocompatible polymers
- Solvents: Ethyl acetate or other Class 3 solvents
- Surfactants: Polyvinyl alcohol (PVA), polysorbates, or poloxamers
- Equipment: Microfluidizer system (Microfluidics Inc.) or equivalent high-pressure homogenizer
Procedure:
Initial Emulsion Formation:
- Dissolve polymer and drug in organic solvent (e.g., ethyl acetate)
- Prepare aqueous phase containing surfactant (e.g., 1-2% PVA)
- Pre-mix organic and aqueous phases using high-speed homogenizer (10,000 rpm, 2 minutes) to form coarse emulsion
High-Pressure Homogenization:
- Prime Microfluidizer system with aqueous surfactant solution
- Process coarse emulsion at 15,000-30,000 psi for 5-10 cycles
- Monitor particle size after every 2-3 cycles until target size is achieved
Solvent Removal and Purification:
- Remove organic solvent by stirring under reduced pressure or dialysis
- Concentrate nanoparticles by ultrafiltration
- Wash to remove excess surfactant and free drug
Critical Parameters:
- Homogenization pressure: Directly affects particle size and distribution
- Number of cycles: Typically 5-15 cycles required for size reduction
- Surfactant type and concentration: Critical for stability and final particle size
- Temperature control: Important for heat-labile compounds
Diagram 1: Microfluidizer nanoparticle production workflow. This continuous process enables scalable production with precise size control.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful scale-up of PNP production requires careful selection of materials and reagents that balance performance with regulatory and manufacturing considerations. Table 3 details key research reagent solutions and their functions in scale-up production.
Table 3: Essential Research Reagent Solutions for PNP Scale-Up
| Reagent Category | Specific Examples | Function in Formulation | Scale-Up Considerations |
|---|---|---|---|
| Biodegradable Polymers | PLGA, PCL, PLA [54] [17] | Form nanoparticle matrix; Control drug release rate [17] | Commercial availability; Regulatory acceptance; Batch consistency [8] |
| Surface Stabilizers | PVA, Poloxamer 188, PEG [54] [8] | Prevent aggregation; Modify surface properties [54] | Quality grades; Concentration optimization; Purification requirements [8] |
| Organic Solvents | Ethyl acetate, Acetonitrile [54] [78] | Dissolve polymer and drug; Form organic phase [54] | Residual solvent limits; Toxicity profile; Removal efficiency [78] |
| Targeting Ligands | Peptides, Antibodies, Folate [8] [6] | Enable active targeting to specific cells/tissues [8] | Conjugation efficiency; Stability during storage; Cost at scale [8] |
| Cryoprotectants | Trehalose, Sucrose, Mannitol [78] | Stabilize during freeze-drying; Prevent aggregation [78] | Optimization of type and concentration; Impact on reconstitution [78] |
Diagram 2: Integrated strategy for successful PNP scale-up. This approach balances material selection, process design, and quality control.
Characterization and Quality Control for Scale-Up
Robust characterization throughout the scale-up process is essential to ensure consistent product quality. The transition from laboratory to industrial scale requires implementation of Quality by Design (QbD) principles and Process Analytical Technologies (PAT) to monitor Critical Quality Attributes (CQAs) in real-time [8]. Key parameters requiring strict control include particle size (typically 10-200 nm for systemic administration), polydispersity index (PDI < 0.2 indicating monodisperse populations), zeta potential (indicating colloidal stability), drug loading capacity, and encapsulation efficiency [31].
Advanced characterization techniques such as diffusion-ordered NMR spectroscopy (DOSY) can provide valuable information about molecular weight and polymer conformation, while automated dynamic light scattering systems enable real-time size monitoring during production [31]. Establishing correlations between process parameters and these CQAs is fundamental to developing a design space for regulatory submission and ensuring product consistency throughout technology transfer to manufacturing facilities.
Bridging the gap between laboratory-scale development and industrial production of polymeric nanoparticles requires a multidisciplinary approach addressing both technical and biological challenges. The integration of continuous manufacturing platforms, such as automated coaxial jet mixing and microfluidics, with robust characterization methodologies represents a promising path forward for overcoming current scale-up limitations [77] [78]. Future advancements will likely focus on increasing process automation, implementing artificial intelligence for predictive modeling and control, and developing novel biodegradable polymers with enhanced functionality [8] [6]. Furthermore, addressing the translational gap requires closer collaboration between formulation scientists, process engineers, and regulatory specialists early in development to ensure that scalable manufacturing remains a primary design consideration rather than an afterthought. By adopting the systematic approaches outlined in this Application Note, researchers can significantly enhance the likelihood of successfully translating promising PNP formulations from bench to bedside.
Stimuli-responsive polymeric nanoparticles (PNPs) represent a groundbreaking advancement in nanomedicine, offering unprecedented control over therapeutic delivery. These intelligent systems are engineered to respond to specific biochemical or physical triggers, enabling precise drug release at the target site while minimizing off-target effects [12] [79]. The foundation of their design lies in the versatile properties of polymeric materials, which can be tailored to exhibit dramatic changes in conformation, solubility, or degradation profile upon encountering pathological stimuli [80]. This capability transforms conventional PNPs from passive carriers into active participants in therapeutic intervention, creating a new paradigm for treating complex diseases, particularly cancer, where the tumor microenvironment presents multiple distinctive biochemical signals [81] [82].
The intelligence of these systems stems from their multifunctional architecture, which integrates targeting ligands, environment-sensing elements, and controlled-release mechanisms within a single nanoscale platform [49] [79]. Recent advances in polymer chemistry and nanotechnology have accelerated the development of these sophisticated systems, with innovations ranging from polymer-drug conjugates to complex hybrid nanostructures capable of integrating diagnostic and therapeutic functions (theranostics) [12] [49]. As the field progresses toward clinical translation, standardized protocols for the fabrication and evaluation of stimuli-responsive PNPs become increasingly critical for ensuring reproducibility, efficacy, and safety [83] [84].
Stimuli-Responsive Mechanisms: Quantitative Analysis of Triggering Modalities
Stimuli-responsive PNPs are classified based on their triggering mechanisms, which can be endogenous (originating from pathological conditions) or exogenous (externally applied). The quantitative characterization of these triggers provides critical parameters for rational PNP design, influencing decisions regarding polymer selection, nanoparticle architecture, and triggering thresholds.
Table 1: Endogenous Stimuli-Responsive Systems
| Stimulus Type | Typical Trigger Parameters | Common Polymer Systems | Responsive Mechanism | Drug Release Kinetics |
|---|---|---|---|---|
| pH | Tumor microenvironment: pH 6.5-7.0; Endosomes: pH 5.0-6.0 [80] | Poly(lactic-co-glycolic acid), Chitosan, Poly(β-amino esters) [80] [84] | Protonation, hydrolysis, acetal/ortho ester cleavage [80] | 50-90% release within 2-48h at target pH [80] |
| Redox (GSH) | Intracellular GSH: 2-10 mM; Extracellular GSH: 2-20 μM [80] [82] | Disulfide-containing polymers, Poly(γ-glutamic acid) [80] | Disulfide bond reduction and nanoparticle disassembly [80] [82] | >80% release within 12-24h in reducing environments [80] |
| Enzymes | Overexpressed proteases (MMPs, cathepsins) in tumor microenvironment [80] [82] | Peptide-polymer conjugates, Poly(amino acids) [80] | Enzyme-specific substrate cleavage [80] | Protease-dependent; typically 60-95% release within 4-48h [80] |
Table 2: Exogenous Stimuli-Responsive Systems
| Stimulus Type | Typical Application Parameters | Common Polymer Systems | Responsive Mechanism | Activation Characteristics |
|---|---|---|---|---|
| Light (NIR) | 650-900 nm wavelength; 0.5-2.0 W/cm² intensity [80] [82] | Polymers conjugated with photosensitizers (e.g., indocyanine green) [80] | Photothermal heating or photochemical cleavage [80] [79] | Spatial precision: 1-2 mm; Temporal control: seconds to minutes [80] |
| Temperature | Hyperthermia: 40-45°C; Local heating [80] [82] | Poly(N-isopropylacrylamide), Pluronics [80] | Phase transition (swelling/collapse) at lower critical solution temperature [80] | Reversible on/off release; typically 2-5-fold increase in release rate [80] |
| Ultrasound | 1-3 MHz frequency; 0.5-3.0 W/cm² intensity [80] [82] | Microbubble-PNP conjugates, Perfluorocarbon-loaded PNPs [80] | Cavitation-induced membrane permeabilization or thermal effects [80] | Deep tissue penetration (up to 10 cm); temporal control: minutes [80] |
Application Note: Optimizing pH-Responsive Systems for Tumor Targeting
The slightly acidic tumor microenvironment (pH 6.5-7.0) and progressively acidic endo-lysosomal compartments (pH 5.0-6.0) provide a physiological gradient for targeted drug release [80]. pH-responsive PNPs utilizing poly(β-amino esters) or acetal-based polymers demonstrate accelerated drug release under acidic conditions, with studies showing 2-5 fold increased cytotoxicity in cancer cells compared to non-responsive controls [80]. The incorporation of pH-sensitive elements along with targeting ligands (e.g., folic acid, transferrin) creates dual-targeting systems that synergistically enhance tumor-specific accumulation through both active targeting and microenvironment responsiveness [12] [79].
Fabrication Protocols for Stimuli-Responsive PNPs
Protocol: Nanoprecipitation of pH-Redox Dual-Responsive PNPs
This protocol describes the synthesis of PNPs responsive to both acidic pH and elevated glutathione (GSH) levels, suitable for targeted cancer therapy [80] [84].
Materials:
- Polymer: PLGA-PEG-ss-PEI (synthesized with disulfide linkages)
- Drug: Doxorubicin hydrochloride
- Solvents: Acetone (HPLC grade), Dimethyl sulfoxide (DMSO)
- Purification: Amicon Ultra centrifugal filters (100 kDa MWCO)
- Characterization: Dynamic light scattering (DLS), HPLC system
Procedure:
- Organic Phase Preparation: Dissolve 50 mg PLGA-PEG-ss-PEI polymer and 5 mg doxorubicin in 10 mL acetone. Stir for 30 minutes at 600 rpm until completely dissolved.
- Aqueous Phase Preparation: Add 20 mL of deionized water to a 50 mL beaker maintained at 25°C with continuous magnetic stirring at 800 rpm.
- Nanoprecipitation: Inject the organic phase into the aqueous phase rapidly using a syringe pump at a rate of 1 mL/min. Immediate nanoparticle formation occurs.
- Solvent Removal: Stir the nanoparticle suspension for 4 hours to allow complete evaporation of organic solvent.
- Purification: Concentrate the nanoparticles using Amicon Ultra centrifugal filters (100 kDa MWCO) at 4000 × g for 10 minutes. Wash three times with deionized water to remove unencapsulated drug.
- Characterization:
- Size and Zeta Potential: Dilute purified nanoparticles 1:10 in PBS and analyze using DLS.
- Drug Loading: Dissolve 1 mg nanoparticles in DMSO and quantify doxorubicin content via HPLC (λex=480 nm, λem=560 nm).
- Encapsulation Efficiency (EE%) = (Actual drug loading / Theoretical drug loading) × 100
Expected Outcomes:
- Particle size: 80-150 nm with PDI < 0.2
- Zeta potential: +15 to +25 mV (due to PEI segment)
- Drug loading: 5-8% (w/w)
- Encapsulation efficiency: >70%
- Stimuli-responsive release: <20% release at pH 7.4 in 24h; >60% release at pH 5.0 with 10 mM GSH
Protocol: Emulsion-Solvent Evaporation for Thermo-Responsive PNPs
This method produces temperature-sensitive PNPs based on poly(N-isopropylacrylamide) (PNIPAAm) for thermally-triggered drug release [80] [84].
Materials:
- Polymer: PLGA-PNIPAAm block copolymer
- Drug: Paclitaxel or other hydrophobic chemotherapeutic
- Solvents: Dichloromethane (DCM), Polyvinyl alcohol (PVA, 1% w/v)
- Equipment: Probe sonicator, Rotary evaporator
Procedure:
- Organic Phase: Dissolve 50 mg PLGA-PNIPAAm and 5 mg paclitaxel in 5 mL DCM.
- Aqueous Phase: Prepare 50 mL of 1% PVA solution.
- Primary Emulsion: Add organic phase to aqueous phase and emulsify using probe sonication (50% amplitude, 2 minutes pulse mode: 10s on/5s off) in an ice bath.
- Solvent Evaporation: Transfer emulsion to round-bottom flask and evaporate DCM using rotary evaporator (200 mbar, 37°C, 30 minutes).
- Collection: Centrifuge nanoparticles at 15,000 × g for 20 minutes and wash twice with deionized water.
- Lyophilization: Resuspend in 5% trehalose solution and freeze-dry for 48 hours for long-term storage.
Expected Outcomes:
- Particle size: 100-200 nm
- Lower Critical Solution Temperature (LCST): 32-37°C (tunable via copolymer composition)
- Drug release: <15% at 37°C; >60% at 42°C over 24h
- Applications: Hyperthermia-mediated cancer therapy
Visualization of Stimuli-Responsive Mechanisms
The following diagrams illustrate key mechanisms and experimental workflows for stimuli-responsive PNPs.
Diagram 1: Stimuli-Responsive Mechanisms in PNPs. This diagram illustrates the endogenous and exogenous triggers that can be leveraged for controlled drug release from intelligent PNPs.
Diagram 2: Experimental Workflow for PNP Development. This diagram outlines the standardized process for fabricating, characterizing, and evaluating stimuli-responsive PNPs.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Stimuli-Responsive PNP Development
| Category | Specific Reagents/Materials | Function/Application | Key Considerations |
|---|---|---|---|
| Polymer Systems | PLGA, PLA, PCL, Chitosan, Poly(β-amino esters), PNIPAAm [80] [84] | Backbone materials providing structural integrity and stimulus responsiveness | Biodegradability, biocompatibility, functional groups for modification, regulatory status (FDA-approved) |
| Stimuli-Responsive Elements | Disulfide linkers, Acetal/ortho ester groups, pH-sensitive peptides, Photochromic compounds [80] [82] | Enable triggered response to specific stimuli (pH, redox, enzymes, light) | Trigger specificity, response kinetics, stability during circulation |
| Targeting Ligands | Folic acid, Transferrin, Antibodies, Peptides (RGD), Aptamers [12] [79] | Enhance specific accumulation in target tissues via active targeting | Binding affinity, density on nanoparticle surface, potential immunogenicity |
| Characterization Tools | Dynamic Light Scattering, HPLC systems, Dialysis membranes, Fluorescence spectroscopy [12] [84] | Quantify nanoparticle properties, drug loading, and release kinetics | Accuracy, sensitivity, reproducibility across experimental batches |
| Biological Assay Reagents | Cell culture media, MTT/XTT assay kits, Lysotracker dyes, ELISA kits for cytokine profiling [83] [79] | Evaluate cellular uptake, cytotoxicity, and immune response | Compatibility with nanoparticle systems, appropriate controls, quantitative reliability |
Stimuli-responsive PNPs represent the forefront of intelligent drug delivery system design, offering sophisticated solutions to the challenges of targeted therapy. The protocols and application notes provided herein establish a framework for the standardized development and evaluation of these systems, with quantitative parameters serving as benchmarks for performance optimization. As the field advances, the integration of artificial intelligence in nanoparticle design, along with improved understanding of biological barriers, will further enhance the precision and clinical applicability of these intelligent systems [12] [79]. The ongoing transition from conventional nanocarriers to smart, responsive platforms heralds a new era of personalized medicine with the potential to significantly improve therapeutic outcomes across numerous disease states.
Optimizing Drug Loading Capacity and Controlling Release Kinetics
In the development of polymeric nanoparticle (PNP)-based drug delivery systems, two parameters are critically important for therapeutic efficacy: drug loading capacity and release kinetics. Optimizing these factors is essential to enhance the therapeutic index of medications, minimize side effects, and achieve targeted delivery. Polymeric nanoparticles offer significant advantages over conventional drug delivery systems, including improved drug stability, enhanced bioavailability, and the potential for controlled and targeted release [12] [31]. Their versatility allows for the encapsulation of diverse therapeutic agents, from small molecules to complex biologics [9]. However, challenges remain in achieving high drug loading and precise control over release profiles. This Application Note provides detailed protocols and data-driven strategies to address these challenges, enabling researchers to design more effective nanomedicines.
Quantitative Analysis of Factors Influencing Drug Loading and Release
Key Factors Affecting Drug Loading Capacity (LC) and Encapsulation Efficiency (EE)
| Factor | Impact on LC/EE | Quantitative Evidence & Mechanisms |
|---|---|---|
| Drug-Polymer Solubility & Interactions | Primary influence on LC. | A pseudo-constant K* characterizes drug-polymer interaction intensity. Drugs with higher K* (e.g., Clofazimine, Sorafenib) show stronger interactions, though solubility in the solvent system is the key determinant for final LC [85]. |
| Drug Lipophilicity (Log P) | Moderate positive correlation with EE. | Analysis of a PLGA nanoparticle dataset revealed a moderate positive correlation between the drug's Log P and its encapsulation efficiency [62]. |
| Drug to Polymer Ratio (D:P) | Strong positive correlation with LC. | A comprehensive analysis of 433 PLGA formulations identified a strong positive correlation between the D:P ratio and the final loading capacity of the nanoparticles [62]. |
| Polymer Composition | Influences particle properties and LC. | For PLGA, the Lactide to Glycolide (LA:GA) ratio shows a moderate correlation with nanoparticle size, which can indirectly affect loading [62]. Chitosan's degree of deacetylation and molecular weight significantly impact its physical properties and drug loading capabilities [86]. |
| Formulation Method | Affects LC, EE, and particle size. | Methods like nanoprecipitation, ionic cross-linking, and emulsion-based techniques yield nanoparticles with different characteristics. The choice of stabilizer (e.g., TPGS) is also critical [44] [86]. |
Key Factors Affecting Drug Release Kinetics
| Factor | Impact on Release Kinetics | Quantitative Evidence & Mechanisms |
|---|---|---|
| Polymer Erosion & Degradation | Controls sustained release. | Biodegradable polymers like PLGA and Chitosan undergo hydrolysis, providing a slow, controlled release mechanism. The degradation half-time of Chitosan NPs can range from days to several weeks [86]. |
| Stimuli-Responsive Design | Enables precise, triggered release. | "Smart" PNPs can be engineered to respond to specific stimuli (e.g., pH, temperature, enzymes) at the target site, enhancing precision and minimizing off-target effects [12]. |
| Surface Functionalization | Modulates release profile and targeting. | PEGylation minimizes non-specific interactions and can prolong circulation. The addition of targeting ligands (e.g., antibodies, peptides, folates) enables active targeting [12]. |
| Nanoparticle Architecture | Provides fine control over release rate. | Layer-by-Layer (LbL) assembly allows for exquisite control over shell composition and thickness. Studies show that varying the ratio of polyelectrolytes (e.g., CMS:SS from 1:2 to 1:8) can reduce premature drug release in the upper GI tract from 60% to 12% [9]. |
Experimental Protocols
Protocol 1: Preparation of Polymeric Nanoparticles via Flash Nanoprecipitation
Application: For efficient encapsulation of poorly water-soluble drugs. Principle: This method utilizes rapid mixing of an organic solvent stream containing the drug and polymer with an anti-solvent (aqueous) stream, leading to instantaneous nanoparticle precipitation with high drug loading [44] [85].
Materials:
- Polymer: PLGA or a similar biodegradable polymer.
- Stabilizer: D-α-tocopheryl polyethylene glycol 1000 succinate (TPGS), Polyvinyl Alcohol (PVA).
- Drug: A poorly water-soluble model drug (e.g., Itraconazole, Sorafenib).
- Organic Solvent: Acetone, Ethanol, or Dimethylformamide (DMF).
- Equipment: Custom-made or commercial multi-inlet vortex mixer (MIVM), syringe pumps.
Procedure:
- Prepare Streams:
- Inlet 1 (Organic Phase): Dissolve the drug and polymer in a suitable organic solvent.
- Inlets 2-4 (Aqueous Phase): Use water, which may contain a stabilizer like 0.05% w/v PVA.
- Set Flow Rates: Configure syringe pumps to control the flow. A typical setup uses 10 mL/min for the organic stream (Inlet 1) and 90 mL/min for the aqueous streams (Inlets 2-4) to achieve a final organic solvent concentration of 5% v/v.
- Mix and Collect: Rapidly mix the streams in the MIVM. Ensure the Reynolds number (Re) is >4000 to achieve turbulent flow and efficient mixing. Collect the nanoparticle suspension from the outlet.
- Purify: Use dialysis or tangential flow filtration to remove organic solvents and free, unencapsulated drug.
Protocol 2: Advanced In Vitro Release Study Using Centrifugal Ultrafiltration
Application: Accurate determination of drug release kinetics from nanoparticles. Principle: This Sample and Separate (SS) method combines USP Apparatus II (paddle) with centrifugal ultrafiltration (CU) to efficiently separate released free drug from the nanoparticles, providing a more accurate release profile than traditional dialysis [44].
Materials:
- Release Medium: A suitable buffer (e.g., PBS) with surfactants (e.g., 0.5% w/v SDS) to maintain sink conditions.
- Equipment: USP Dissolution Apparatus II (Paddle), centrifuge, centrifugal ultrafiltration devices (e.g., Amicon Ultra with appropriate MWCO).
- HPLC System: For quantifying drug concentration.
Procedure:
- Confirm Sink Conditions: Prior to the study, determine the drug's solubility in the selected release medium. The volume of the medium must be at least three times that required to form a saturated solution.
- Initiate Release Study: Place the nanoparticle suspension in the vessel of USP Apparatus II. Maintain the temperature at 37±0.5°C and the paddle speed at 50-100 rpm.
- Sample at Time Intervals: At predetermined time points, withdraw a known volume of the release medium.
- Separate Free Drug: Immediately process the sample using a centrifugal ultrafiltration device. Centrifuge according to the device specifications (e.g., 14,000 × g for 10 minutes). The free drug will be in the filtrate, while the nanoparticles are retained.
- Quantify Drug: Analyze the filtrate using HPLC to determine the concentration of the released drug.
- Data Analysis: Plot the cumulative drug release over time and fit the data to mathematical models (e.g., Higuchi, Korsmeyer-Peppas) to understand the release mechanism.
Protocol 3: Direct Quantification of Drug Loading Using ATR-FTIR Spectroscopy
Application: Direct, reliable measurement of drug loading content (DLC) without extensive sample preparation. Principle: Attenuated total reflection Fourier transform infrared (ATR-FTIR) spectroscopy can directly quantify the drug in nanoparticle dispersions by measuring characteristic infrared absorption bands, overcoming issues of incomplete drug extraction [87].
Materials:
- Model System: Silk fibroin nanoparticles (SFN) loaded with Naringenin (NAR).
- Equipment: ATR-FTIR Spectrometer.
Procedure:
- Calibration Curve:
- Prepare a series of calibration samples with known, increasing masses of NAR and a constant mass of SFN.
- Disperse the mixtures in a 30% ethanol solution to ensure homogeneity.
- Acquire the FTIR spectrum for each calibration standard.
- Identify a unique absorption band for NAR and plot its intensity (e.g., peak height or area) against the known NAR concentration to create a calibration curve.
- Sample Measurement:
- Prepare your drug-loaded nanoparticle sample.
- Record its FTIR spectrum under the same conditions as the calibration standards.
- Measure the intensity of the characteristic drug peak.
- Calculate DLC: Use the calibration curve to determine the drug content in your unknown sample. Calculate the Drug Loading Content (DLC) and Encapsulation Efficiency (EE) using the formulas:
- DLC (%) = (Weight of drug in nanoparticle / Weight of drug-loaded nanoparticle) × 100
- EE (%) = (Weight of drug in nanoparticle / Weight of drug used in formulation) × 100 [87]
Visualization of Mechanisms and Workflows
Controlled Release Mechanisms
Nanoparticle Preparation and Characterization Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in PNP Development |
|---|---|
| PLGA (Poly(lactic-co-glycolic acid)) | A biodegradable, biocompatible copolymer that forms the nanoparticle matrix. The LA:GA ratio can be tuned to control degradation and release kinetics [62]. |
| Chitosan | A natural, cationic, biodegradable polysaccharide known for its mucoadhesive properties, useful for oral and mucosal delivery [86]. |
| TPGS (D-α-tocopheryl PEG succinate) | A widely used stabilizer and emulsifier in nanoprecipitation that improves nanoparticle stability and can inhibit P-glycoprotein to overcome drug resistance [44]. |
| PVA (Polyvinyl Alcohol) | A stabilizer and surfactant used in emulsion and nanoprecipitation methods to control particle size and prevent aggregation [44]. |
| Centrifugal Ultrafiltration Devices | Essential for the efficient separation of free drug from nanoparticles during in vitro release studies and for determining encapsulation efficiency [44]. |
| Layer-by-Layer (LbL) Polyelectrolytes | Oppositely charged polymers (e.g., Heparin, Polystyrene sulfonate) assembled in layers on a nanoparticle core to provide precise, programmable control over drug release [9]. |
Clinical Translation and Competitive Landscape: Efficacy, Safety, and Market Position
Within the broader context of research on polymeric nanoparticle drug delivery systems, the clinical success of formulations like Abraxane and Genexol-PM represents pivotal validation of nanocarrier strategies. These nanoformulations address fundamental challenges in oncology drug delivery, particularly the poor aqueous solubility and dose-limiting toxicities of potent chemotherapeutic agents [88] [75]. By leveraging nanoscale platforms, these systems have demonstrated improved pharmacokinetic profiles, enhanced tumor accumulation through both passive and active targeting mechanisms, and reduced systemic side effects, thereby establishing new therapeutic paradigms in cancer treatment [89]. This document provides a detailed analysis of these success stories through structured data comparison, experimental protocols, and visualization of key mechanisms to support further research and development in the field.
Quantitative Analysis of Approved Nanoformulations
The following tables summarize key physicochemical characteristics, clinical performance metrics, and approval statuses for selected clinically successful nanoformulations.
Table 1: Physicochemical Properties and Clinical Indications of Key Nanoformulations
| Formulation Name | Nanoparticle Type | Active Compound | Polymer/Carrier Composition | Key Indications | Year Approved |
|---|---|---|---|---|---|
| Abraxane | Protein Nanoparticle | Paclitaxel | Albumin | Breast Cancer, NSCLC, Pancreatic Cancer [89] | 2005 (FDA) [90] |
| Genexol-PM | Polymeric Micelle | Paclitaxel | PEG-PLA diblock copolymer [88] | Breast Cancer, NSCLC [89] | 2007 (South Korea) |
| Doxil | Liposome | Doxorubicin | PEGylated phospholipids [91] | Kaposi's Sarcoma, Ovarian Cancer, Multiple Myeloma [90] | 1995 (FDA) [90] |
| Zilretta | Polymeric Microsphere | Triamcinolone acetonide | PLGA matrix [90] | Osteoarthritis knee pain [90] | 2017 (FDA) [90] |
Table 2: Clinical Performance and Pharmacokinetic Metrics
| Formulation | Key Clinical Benefits | Maximum Tolerated Dose | Notable Adverse Events |
|---|---|---|---|
| Abraxane | Higher tumor uptake vs. solvent-based PTX; allows higher PTX doses with fewer side effects [89] | 100 mg/m² (days 1,8,15 of 21-day cycle for NSCLC with carboplatin) [89] | Reduced neurotoxicity vs. cremophor-based PTX [89] |
| Genexol-PM | Enhanced antitumor activity with cisplatin; higher PTX dosing possible [89] | 180 mg/m² (weekly) [89] | Severe side effects noted with gemcitabine combination [89] |
| Doxil | Reduced cardiotoxicity vs. free doxorubicin; prolonged circulation time [88] [91] | Varies by indication | Palmar-plantar erythrodysesthesia (hand-foot syndrome) [91] |
Experimental Protocols
Protocol: Formulation and Characterization of Albumin-Bound Nanoparticles (Abraxane Model)
Objective: To prepare and characterize albumin-bound paclitaxel nanoparticles using the nab-technology platform.
Materials:
- Paclitaxel (active pharmaceutical ingredient)
- Human serum albumin (HSA)
- High-pressure homogenizer
- Lyophilizer
- Phosphate-buffered saline (PBS), pH 7.4
- Dynamic light scattering (DLS) instrument
- Transmission electron microscope (TEM)
Procedure:
- Solution Preparation: Prepare 1% (w/v) HSA solution in PBS and filter through a 0.22 μm membrane.
- Drug Suspension: Suspend paclitaxel in the HSA solution at a drug-to-albumin ratio of 1:9 to form a coarse suspension.
- High-Pressure Homogenization: Process the suspension through a high-pressure homogenizer at 20,000-30,000 psi for 6 cycles while maintaining temperature below 25°C.
- Sterile Filtration: Filter the resulting nanosuspension through a 0.22 μm membrane under aseptic conditions.
- Lyophilization: Fill vials with the nanosuspension and lyophilize to obtain sterile, pyrogen-free powder.
- Characterization:
- Particle Size Analysis: Dilute the reconstituted formulation 1:100 with Milli-Q water and analyze by DLS. Acceptable specification: 120-150 nm with PDI <0.2.
- Morphology: Examine by TEM after negative staining with 1% uranyl acetate.
- Drug Loading: Determine by HPLC after dissolving nanoparticles in acetonitrile.
Validation Criteria: Mean particle size <150 nm; PDI <0.2; sterility testing per USP <71>; endotoxin levels <5 EU/mg [89].
Protocol: Preparation and Evaluation of Polymeric Micelles (Genexol-PM Model)
Objective: To prepare PEG-PLA diblock copolymer micelles loaded with paclitaxel using the solvent evaporation method.
Materials:
- Paclitaxel
- Methoxy-PEG-PLA diblock copolymer (MW: PEG 2000 Da, PLA 1750 Da)
- Acetonitrile (HPLC grade)
- Dialysis membrane (MWCO 12-14 kDa)
- Dynamic light scattering instrument
- Ultracentrifuge
Procedure:
- Organic Phase Preparation: Dissolve 10 mg paclitaxel and 100 mg PEG-PLA copolymer in 5 mL acetonitrile.
- Aqueous Phase Preparation: Add 20 mL deionized water to a beaker under magnetic stirring at 500 rpm.
- Micelle Formation: Slowly add the organic phase dropwise to the aqueous phase over 10 minutes.
- Solvent Removal: Stir the mixture for 4 hours at room temperature to evaporate organic solvent.
- Purification: Transfer the micellar solution to a dialysis membrane and dialyze against deionized water for 6 hours to remove unencapsulated drug.
- Concentration: Concentrate the micellar solution using rotary evaporation or ultrafiltration.
- Characterization:
- Particle Size and Zeta Potential: Measure by dynamic light scattering.
- Drug Loading: Determine paclitaxel content by HPLC after disrupting micelles with acetonitrile.
- Encapsulation Efficiency: Calculate as (actual loading/theoretical loading) × 100%.
Validation Criteria: Mean particle size <50 nm; PDI <0.2; encapsulation efficiency >85%; drug loading >10% [88].
Visualization of Key Mechanisms and Workflows
Nab-Technology Nanoparticle Formation and Targeting
Diagram 1: Nab-Technology Workflow and Targeting Mechanism. This illustrates the process from formulation to tumor targeting of albumin-bound nanoparticles, highlighting key mechanisms including EPR effect and receptor-mediated transcytosis [89].
Polymeric Micelle Assembly and Drug Delivery Pathway
Diagram 2: Polymeric Micelle Assembly and Delivery Pathway. This depicts the self-assembly process of polymeric micelles and their subsequent journey through circulation, tumor accumulation via EPR effect, and cellular drug release [88].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Nanoformulation Development
| Reagent/Chemical | Function/Application | Example Usage in Protocols |
|---|---|---|
| Human Serum Albumin (HSA) | Natural carrier protein for hydrophobic drugs; facilitates receptor-mediated transport [89] | Formulation of albumin-bound nanoparticles (Abraxane model) |
| PEG-PLA Diblock Copolymer | Amphiphilic polymer for micelle formation; provides steric stabilization and drug encapsulation [88] | Preparation of polymeric micelles (Genexol-PM model) |
| High-Pressure Homogenizer | Equipment for producing uniform nanosuspensions through intense shear forces | Particle size reduction in albumin nanoparticle production |
| Dialysis Membrane (MWCO 12-14 kDa) | Purification method to remove unencapsulated drugs and organic solvents | Cleaning polymeric micelle formulations after preparation |
| Dynamic Light Scattering Instrument | Analytical technique for measuring particle size, distribution, and zeta potential | Quality control assessment of final nanoparticle formulations |
The development of polymeric nanoparticles (PNPs) represents a groundbreaking advancement in targeted drug delivery, offering significant benefits over conventional systems through enhanced biocompatibility, controlled release, and improved therapeutic efficacy while minimizing side effects [12]. The versatility of polymers allows for the creation of a virtually limitless range of carriers with finely tuned properties, making them ideal for addressing complex diseases like cancer, autoimmune disorders, and infectious diseases [31] [9]. This application note provides a structured overview of the current clinical pipeline for PNP-based therapies, summarizes key quantitative data for comparison, details essential experimental protocols for nanoparticle characterization, and visualizes critical pathways and workflows to support research and development activities in this rapidly evolving field.
The following table consolidates key information on polymeric nanoparticle-based therapeutics that have advanced to clinical trials, highlighting their applications, stages of development, and notable outcomes.
Table 1: Overview of Polymeric Nanoparticle-Based Therapeutics in Clinical Development
| Therapeutic Name | Polymeric Composition | Therapeutic Agent | Indication | Development Phase | Key Findings/Status |
|---|---|---|---|---|---|
| BIND-014 | PLGA-PEG | Docetaxel | Prostate Cancer, Cholangiocarcinoma, Tonsillar Cancer | Preliminary Clinical Data (Phase I/II) | Shrinkage of metastatic lesions at lower doses (15-30 mg/m²) than solvent-based docetaxel (75 mg/m²) [92]. |
| CRLX101 | Cyclodextrin-based Polymer | Camptothecin | Cancer | Phase I/II/III (Completed/Enrolling) | Clinical trials ongoing to identify benefits/limitations of nanomedicines [92]. |
| NK105 | Polymeric Micelle | Paclitaxel | Cancer | Phase I/II/III (Completed/Enrolling) | Clinical trials ongoing to identify benefits/limitations of nanomedicines [92]. |
| Genexol-PM | PEG-PLA Micelle | Paclitaxel | Cancer | Phase I/II/III (Completed/Enrolling) | Clinical trials ongoing to identify benefits/limitations of nanomedicines [92]. |
| Paclitaxel Polyglumex | Polyglutamic Acid conjugate | Paclitaxel | Non-Small Cell Lung Cancer | Phase III | No significant improvement shown compared to docetaxel as a second-line treatment [92]. |
Experimental Protocols for Characterizing Polymeric Nanoparticles
Rigorous characterization of PNPs is fundamental to understanding their behavior, optimizing their design, and ensuring reproducible performance in preclinical and clinical settings. Below are detailed protocols for key characterization techniques.
Protocol for Nuclear Magnetic Resonance (NMR) Spectroscopy Analysis
Purpose: To confirm polymer structure, monitor polymerization conversion, and quantify drug loading or functional group density in polymer-drug conjugates [31].
Materials:
- Deuterated solvent (e.g., CDCl₃, D₂O)
- NMR tube
- High-resolution NMR spectrometer
Method:
- Sample Preparation: Dissolve approximately 5-10 mg of the purified polymer or polymer-drug conjugate in 0.6 mL of an appropriate deuterated solvent.
- Data Acquisition:
- For structural analysis, run a ¹H NMR experiment. Determine the polymer's chemical structure by analyzing chemical shifts, integration, and splitting patterns.
- For monitoring polymerization, track the disappearance of monomer peaks and the appearance of polymer peaks in sequential ¹H NMR spectra to calculate conversion rates [31].
- For conjugation confirmation, compare the ¹H NMR spectrum of the pristine polymer with that of the final conjugate. The successful linkage is confirmed by the appearance of new characteristic peaks or shifts in existing peaks corresponding to the conjugated drug or dye [31].
- Quantification:
- Drug Loading: Use quantitative ¹H NMR (qNMR) by comparing the integration of a characteristic peak from the conjugated drug to a characteristic peak from the polymer backbone. This allows for the precise calculation of drug loading capacity or the density of functional groups [31].
- Advanced Techniques: Employ two-dimensional NMR techniques (e.g., COSY, HSQC, HMBC) to gain deeper insights into the local chemical environment and confirm the specific site of conjugation [31].
Protocol for Dynamic Light Scattering (DLS) and Zeta Potential Analysis
Purpose: To determine the hydrodynamic diameter, size distribution (polydispersity index, PDI), and surface charge (zeta potential) of PNPs in suspension [9].
Materials:
- Nanoparticle suspension in aqueous buffer
- Disposable zeta cell or cuvette
- Dynamic Light Scattering instrument with zeta potential capability
Method:
- Sample Preparation: Dilute the PNP suspension with an appropriate aqueous buffer (e.g., 1 mM KCl) to a concentration that avoids multiple scattering effects, typically yielding a count rate within the instrument's recommended range.
- Size Measurement:
- Transfer the diluted sample into a disposable sizing cuvette.
- Equilibrate the sample in the instrument for 2 minutes at 25°C.
- Perform the DLS measurement. The instrument will report the hydrodynamic diameter (Z-average) and the PDI, which indicates the breadth of the size distribution.
- Zeta Potential Measurement:
- Transfer the diluted sample into a disposable zeta cell.
- Equilibrate the sample in the instrument for 2 minutes at 25°C.
- Measure the zeta potential, which is determined by the electrophoretic mobility of the particles in an applied electric field. A high positive or negative zeta potential (typically > |±30| mV) indicates good colloidal stability.
- Data Interpretation: Report the Z-average diameter, PDI, and zeta potential as the mean ± standard deviation from at least three independent measurements.
Visualization of Pathways and Workflows
Rational Design Workflow for Polymeric Nanoparticles
The following diagram illustrates the logical workflow for the rational design and optimization of polymeric nanoparticles for biologic delivery, integrating key considerations from synthesis to functional assessment.
Rational Design Workflow
Mechanism of Active Tumor Targeting
This diagram outlines the key signaling pathways and biological mechanisms involved in the active targeting of tumors by ligand-functionalized polymeric nanoparticles.
Active Tumor Targeting
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for the formulation, characterization, and functional testing of polymeric nanoparticles for drug delivery.
Table 2: Essential Research Reagents and Materials for Polymeric Nanoparticle Development
| Reagent/Material | Function/Application | Examples / Key Characteristics |
|---|---|---|
| Biodegradable Polymers | Form the nanoparticle matrix; determine biodegradability, compatibility, and release kinetics. | PLGA (FDA-approved), Poly(lactic acid) (PLA), Chitosan (natural polymer) [12] [11]. |
| Functional Polymers | Enable "smart," stimuli-responsive release or enhance stability and circulation time. | PEG (for PEGylation to enhance stability), pH- or temperature-responsive polymers [12] [31]. |
| Targeting Ligands | Actively direct nanoparticles to specific cells or tissues, enhancing therapeutic precision. | Antibodies, Peptides, Folates [12]. |
| Surfactants & Stabilizers | Act as stabilizers during nanoemulsion formulation; prevent aggregation. | Polyvinyl Alcohol (PVA), Poloxamers (e.g., Pluronic F127) [11]. |
| Characterization Standards | Provide benchmarks for sizing, concentration, and surface charge measurements. | Latex beads for DLS calibration, standard solutions for zeta potential measurement [31]. |
Nanocarriers have revolutionized contemporary medicine by improving the bioavailability, targeting, and controlled release of therapeutic agents [75]. Among the diverse array of nanocarriers, polymeric nanoparticles (PNPs), lipid-based nanoparticles, and inorganic nanoparticles represent the most extensively researched categories, each offering distinct advantages and limitations for drug delivery applications [93] [94]. This analysis provides a systematic comparison of these nanocarrier systems, focusing on their physicochemical properties, drug delivery capabilities, and therapeutic applications. Framed within a broader thesis on polymeric nanoparticle drug delivery systems, this document offers detailed experimental protocols and application notes tailored for researchers, scientists, and drug development professionals seeking to select and optimize nanocarriers for specific biomedical applications.
Comparative Analysis of Nanocarrier Properties
The table below summarizes the fundamental characteristics, advantages, and limitations of the three primary nanocarrier classes.
Table 1: Comparative analysis of major nanocarrier systems
| Characteristic | Polymeric Nanoparticles (PNPs) | Lipid-Based Nanoparticles | Inorganic Nanoparticles |
|---|---|---|---|
| Composition | Synthetic (e.g., PLGA, PLA, PEG) and natural (e.g., chitosan, hyaluronic acid) polymers [93] [11] | Lipids, phospholipids, cholesterol [93] | Metals (e.g., gold, iron oxide), carbon-based materials, silica [93] [95] |
| Key Advantages | High versatility, controlled release profiles, superior stability, ease of surface functionalization, biocompatibility and biodegradability (for many polymers) [93] [6] | High biocompatibility, ability to encapsulate both hydrophilic and hydrophobic drugs, clinical validation (e.g., in mRNA vaccines) [93] [96] | Unique optical, magnetic, and electronic properties; high contrast for imaging (theranostics); efficient photothermal conversion [93] [95] |
| Primary Limitations | Potential toxicity concerns with some synthetic polymers; complexity in scalable manufacturing [93] [6] | Relatively lower drug loading capacity for some types; stability issues (e.g., oxidation, fusion) [93] | Poor biodegradability leading to potential long-term accumulation; toxicity concerns for some metals [93] |
| Drug Loading & Release | High drug loading capacity; controlled release kinetics via polymer degradation/diffusion; stimuli-responsive designs possible [93] [6] | Encapsulation within lipid bilayer or core; release governed by diffusion and carrier degradation [93] | Typically surface adsorption or conjugation; release can be triggered by external stimuli (e.g., light, magnetic field) [93] |
| Targeting Mechanisms | Passive (EPR effect) and active targeting (via surface ligands like antibodies, peptides); enhanced penetration via PEGylation [6] | Passive targeting via EPR effect; surface functionalization for active targeting possible [94] | Passive targeting; active targeting through surface ligand functionalization [95] |
| Key Applications | Cancer therapy, ocular delivery, nutraceutical delivery, gene therapy [11] [94] | mRNA/siRNA delivery, cancer therapy, vaccines [94] [96] | Medical imaging (MRI, CT, photoacoustic), photothermal therapy, hyperthermia, diagnostic sensing [93] [95] |
Experimental Protocols for Nanocarrier Evaluation
Protocol: Formulation and Physicochemical Characterization
Objective: To synthesize PNPs, lipid-based, and inorganic nanocarriers and characterize their fundamental physicochemical properties.
Materials:
- Polymers/Lipids/Metal Salts: PLGA, PEG, ionizable lipids (e.g., MC3), phospholipids, hydrogen tetrachloroaurate (for gold NPs) [93] [96] [6]
- Solvents: Dichloromethane, acetone, ethanol
- Stabilizers: Polyvinyl Alcohol (PVA), surfactants (e.g., Poloxamer) [11]
- Equipment: Probe sonicator, magnetic stirrer, dynamic light scattering (DLS) instrument, transmission electron microscope (TEM)
Methodology:
- Synthesis:
- PNPs: Prepare using nanoprecipitation or emulsion-solvent evaporation methods. Dissolve polymer and drug in organic solvent, then emulsify in aqueous phase containing stabilizer. Evaporate solvent to form solid nanoparticles [93] [11].
- Lipid Nanoparticles (LNPs): Utilize microfluidic mixing. Combine lipid mixture dissolved in ethanol with aqueous phase (e.g., mRNA in citrate buffer) under controlled flow rates to form self-assembled LNPs [96].
- Gold Nanoparticles (AuNPs): Synthesize by citrate reduction. Boil hydrogen tetrachloroaurate solution and rapidly add sodium citrate solution under stirring until color changes, indicating nanoparticle formation [93].
- Characterization:
- Size and Zeta Potential: Analyze using Dynamic Light Scattering (DLS). Dilute nanocarrier dispersion in purified water and measure to determine hydrodynamic diameter, polydispersity index (PDI), and surface charge [6].
- Morphology: Image using Transmission Electron Microscopy (TEM). Place a drop of diluted nanocarrier suspension on a carbon-coated copper grid, stain if necessary, and air-dry before analysis [6].
- Drug Loading and Encapsulation Efficiency: Separate unencapsulated drug via centrifugation or dialysis. Lyse the purified nanocarriers and quantify drug content using HPLC or UV-Vis spectroscopy. Calculate Encapsulation Efficiency (EE%) and Drug Loading (DL%) [93].
Protocol: Single-Cell Resolution Biodistribution Analysis (SCP-Nano)
Objective: To comprehensively quantify the targeting and biodistribution of nanocarriers throughout a whole organism at single-cell resolution [96].
Materials:
- Fluorescence-labeled nanocarriers (e.g., Alexa Fluor-tagged)
- Mice (appropriate model organism)
- DISCO tissue clearing reagents (without urea and sodium azide) [96]
- Light sheet fluorescence microscope
- High-performance computing resources
Methodology:
- Administration and Tissue Preparation: Administer fluorescently labeled nanocarriers to mice via the desired route (e.g., intravenous, intramuscular). After a predetermined time, perfuse mice transcardially with phosphate-buffered saline (PBS) followed by 4% paraformaldehyde (PFA) [96].
- Whole-Body Tissue Clearing: Subject the entire mouse body to an optimized DISCO clearing protocol. This involves a series of dehydration and delipidation steps while avoiding urea and minimizing dichloromethane incubation to preserve fluorescence signals [96].
- 3D Light-Sheet Microscopy: Image the cleared whole mouse body using light-sheet microscopy at high resolution (approximately 1–2 µm laterally, 6 µm axially) to generate large-scale 3D image datasets of nanocarrier distribution [96].
- AI-Based Image Analysis (SCP-Nano Pipeline):
- Data Partitioning: Partition the whole-body imaging data into manageable 3D patches for deep learning analysis.
- Cell Instance Segmentation: Process the patches using a trained 3D U-Net deep learning model to detect and segment individual targeted cells or nanocarrier clusters accurately.
- Quantification and Mapping: Use the
cc3dlibrary to identify each segmented instance and compute organ-level statistics, including nanocarrier density, size, and intensity contrast relative to the background [96].
Figure 1: SCP-Nano workflow for high-resolution biodistribution mapping.
Protocol: Intracellular Payload Delivery Efficiency Assessment
Objective: To evaluate the ability of nanocarriers to escape endosomal compartments and successfully deliver their payload into the cell cytosol [97].
Materials:
- Genetically engineered mouse cells expressing the Gal8-mRuby fluorescent marker [97]
- Biodegradable nanoparticles carrying fluorescent cargo or mRNA (e.g., encoding luciferase)
- Confocal microscope
- Image analysis software
Methodology:
- Cell Seeding and Transfection: Seed the Gal8-mRuby reporter cells in multi-well plates and allow them to adhere overnight.
- Nanocarrier Treatment: Incubate cells with the test nanocarriers. Include appropriate controls (e.g., untreated cells, cells with nanoparticles known to have poor escape efficiency).
- Imaging and Analysis: After incubation, image the cells using confocal microscopy. The Gal8-mRuby marker fluoresces orange-red when the endosomal envelope is compromised, indicating cargo release.
- Quantification: Use automated image analysis software to quantify two key parameters:
- Nanoparticle Uptake: Measured by the fluorescence signal from the nanoparticle itself.
- Cargo Release Efficiency: Measured by the intensity of the orange-red Gal8-mRuby signal, which correlates with endosomal escape [97].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key reagents and materials for nanocarrier research
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| PLGA | Biodegradable polymer for PNP synthesis; provides controlled release [11] | FDA-approved; tunable degradation rate based on lactic to glycolic acid ratio. |
| Ionizable Lipids | Key component of LNPs for nucleic acid delivery; enables endosomal escape [96] | e.g., MC3; critical for the efficiency of mRNA vaccines and therapies. |
| Polyethylene Glycol (PEG) | Surface functionalization to impart "stealth" properties; reduces opsonization and prolongs circulation half-life [93] [6] | PEGylation is a common strategy to enhance stability and bioavailability. |
| Targeting Ligands | Active targeting to specific cell types or tissues via surface conjugation [6] | Antibodies, peptides (e.g., RGD), folates. Enhances specificity and reduces off-target effects. |
| Fluorescent Dyes (e.g., Alexa Fluor series) | Labeling nanocarriers for tracking and biodistribution studies in vitro and in vivo [96] [97] | Conjugated to the nanocarrier structure or the encapsulated cargo (e.g., mRNA). |
| Gal8-mRuby Reporter Cell Line | Assessing endosomal escape efficiency of nanocarriers [97] | Fluoresces upon endosomal damage, providing a quantitative readout of cytosolic delivery. |
| Stimuli-Responsive Polymers | Enabling "smart" drug release in response to specific triggers in the disease microenvironment [6] | pH-sensitive (e.g., acetal linkages), enzyme-sensitive, or redox-sensitive polymers. |
The comparative analysis underscores that the selection of a nanocarrier system is inherently application-dependent. PNPs offer exceptional versatility and controlled release, lipid-based systems excel in biocompatibility and nucleic acid delivery, and inorganic nanoparticles provide unparalleled functionality in imaging and hyperthermia. The future of nanocarrier development lies in overcoming existing challenges related to biocompatibility, scalability, and precise targeting. Emerging trends point toward the development of smart, stimuli-responsive systems, hybrid nanocarriers combining the strengths of different materials, and the integration of artificial intelligence for design optimization and high-throughput biodistribution analysis, as demonstrated by the SCP-Nano pipeline [96] [6]. These advancements are paving the way for more personalized and effective nanomedicines.
Regulatory Pathways and Considerations for PNP-based Therapeutics
Polymeric Nanoparticles (PNPs) represent a groundbreaking advancement in targeted drug delivery systems, offering significant benefits over conventional therapeutic approaches. These nanoscale particles, typically ranging from 10 to 1000 nanometers, are engineered from polymers to encapsulate therapeutic agents, enhance bioavailability, and facilitate controlled release [31]. Their versatility, biocompatibility, and ability to navigate biological barriers make them particularly valuable for treating complex diseases like cancer and antibiotic-resistant infections [98]. The effectiveness of PNPs is largely determined by their physicochemical properties—including size, shape, surface charge, and drug-loading capacity—which are directly influenced by polymer characteristics and formulation methods [12] [6].
The regulatory landscape for PNPs is complex and continuously evolving. In the United States, the Food and Drug Administration (FDA) oversees their approval, while the European Medicines Agency (EMA) regulates them in the European Union [99]. These frameworks aim to ensure safety, efficacy, and quality while adapting to the unique challenges posed by nanomedicine. For researchers and drug development professionals, understanding these pathways is crucial for successful clinical translation. This document provides a comprehensive overview of regulatory requirements, experimental protocols, and strategic considerations to support the development of PNP-based therapeutics.
Regulatory Framework and Classification
Product Classification and Regulatory Authorities
Determining the correct regulatory classification is a critical first step, as it dictates the applicable approval pathway. PNPs can be categorized as either medicinal products or medical devices based on their primary mechanism of action [99].
- Medicinal Products: Regulated under centralized procedures, these products achieve their principal intended action through pharmacological, immunological, or metabolic (PIM) mechanisms. In the EU, Directive 2001/83/EC provides the definition and framework [99].
- Medical Devices: These products function primarily by physical or mechanical means, even if they incorporate PIM actions that are secondary to their main function [99].
In the United States, the FDA's Center for Drug Evaluation and Research (CDER) or Center for Biologics Evaluation and Research (CBER) may have jurisdiction, with CBER typically reviewing gene therapies and certain novel biologics [100]. The classification can be ambiguous for innovative PNPs, necessitating early regulatory consultation.
Key Regulatory Challenges for PNP-based Therapeutics
Several unique challenges complicate the regulatory approval of PNPs:
- Novel Mechanism of Action: Unlike conventional drugs, PNPs often function by encoding genetic instructions or enabling targeted, controlled release. This novelty means established regulatory precedents may not directly apply, requiring tailored safety and efficacy assessments [100].
- Complexity in Characterization: A thorough understanding of physicochemical properties—such as particle size distribution, surface charge, encapsulation efficiency, and drug release kinetics—is essential but methodologically challenging [31].
- Toxicity and Immunogenicity: Certain PNP formulations may induce unintended immune responses or organ-specific toxicity (e.g., hepatotoxicity), necessitating comprehensive safety profiling [100].
- Manufacturing and Quality Control (CMC): Maintaining consistent quality during manufacturing is difficult due to the complexity of PNP formulations. Variations in polymer composition, drug purity, or encapsulation efficiency can significantly impact product performance [100] [9]. The FDA expects detailed validation data for each production step, especially during scale-up.
Table: Key Regulatory Challenges and Mitigation Strategies for PNP-based Therapeutics
| Regulatory Challenge | Impact on Development | Recommended Mitigation Strategy |
|---|---|---|
| Classification Ambiguity | Uncertainty in regulatory pathway and requirements | Seek early regulatory advice; prepare scientific justification for classification [100] |
| Novel Mechanism of Action | Lack of established preclinical models and endpoints | Conduct comprehensive mechanism of action studies; engage agencies on novel trial designs [100] |
| Complex CMC Requirements | Batch variability, scalability issues | Implement rigorous in-process controls; demonstrate manufacturing consistency [100] [9] |
| Potential Immunogenicity | Safety concerns may halt clinical development | Include immunotoxicity endpoints in preclinical studies; monitor immune responses in trials [100] |
FDA Regulatory Pathway: A Step-by-Step Guide
Navigating the FDA regulatory process requires a strategic approach. The following steps outline the typical journey for an PNP-based investigational product.
Pre-IND (Investigational New Drug) Preparation
A well-structured Pre-IND package forms the foundation for regulatory success. Developers should compile comprehensive data on [100]:
- Product Characterization: This includes detailed information on the polymer and nanoparticle composition, physicochemical properties (size, charge, morphology), encapsulation efficiency, and stability profile.
- Mechanism of Action: Data on target tissues, cellular uptake, and kinetics of therapeutic action (e.g., protein expression for mRNA PNPs).
- Preclinical Studies: Results from in vitro and in vivo studies covering biodistribution, pharmacokinetics, toxicity, and immunogenicity in relevant animal models.
- Chemistry, Manufacturing, and Controls (CMC) Information: Detailed descriptions of the manufacturing process, including drug substance (e.g., mRNA) synthesis, PNP formulation, quality control testing methods, and storage conditions.
FDA Engagement via Pre-IND Meeting
Early engagement with the FDA is highly recommended to de-risk development. A Pre-IND meeting allows sponsors to align with regulatory expectations on [100]:
- The design of nonclinical studies and suitability of proposed endpoints.
- The clinical trial protocol and patient inclusion criteria.
- Safety monitoring plans.
- CMC controls, release specifications, and strategy for demonstrating comparability after process changes.
IND Submission and Clinical Trials
Once the IND is submitted and cleared by the FDA, human trials can begin. PNP-based therapeutics typically follow a phased clinical development approach [100]:
- Phase 1: Focuses on safety, tolerability, and dose-escalation in a small group of subjects. Pharmacokinetics are also assessed.
- Phase 2: Evaluates preliminary efficacy in targeted patient groups and further refines the dosing regimen.
- Phase 3: Large-scale, confirmatory studies that demonstrate efficacy and monitor adverse effects in a broader population.
For rare diseases or urgent indications, adaptive trial designs and the use of surrogate endpoints may be acceptable to accelerate timelines [100].
Expedited Programs and Strategic Designations
The FDA offers several expedited programs to support breakthrough innovations, many of which are applicable to advanced PNP-based therapies [100].
Table: FDA Expedited Programs for PNP-based Therapeutics
| Program | Key Benefit | Eligibility Criteria |
|---|---|---|
| Fast Track | Early and frequent feedback, rolling review of IND | Serious condition with unmet medical need [100] |
| Breakthrough Therapy | Intensive FDA guidance (e.g., senior management involvement) | Preliminary clinical evidence of substantial improvement over available therapies [100] |
| Accelerated Approval | Approval based on a surrogate endpoint reasonably likely to predict clinical benefit | Life-threatening conditions; post-marketing studies required to verify benefit [100] |
| Priority Review | Shorter FDA review time (6 months instead of 10) | Drug application represents a significant improvement in safety or efficacy [100] |
| Platform Technology Designation | Streamlined review for subsequent applications using the same platform | A platform technology is defined as one that is incorporated into, or used in the manufacture of, more than one drug [101] |
The Platform Technology Designation Program, established under Section 506K of the FD&C Act, is particularly relevant for well-characterized PNP systems that can deliver multiple therapeutic payloads. The FDA has identified lipid nanoparticle (LNP) platforms as potential candidates for this program, setting a precedent for other modular nanocarrier systems [101].
Essential Characterization and Preclinical Protocols
Comprehensive Physicochemical Characterization
Rigorous characterization is the cornerstone of PNP development, informing both product design and regulatory submissions. Key parameters and methods include [31]:
- Size and Size Distribution: Typically measured by Dynamic Light Scattering (DLS). A polydispersity index (PDI) below 0.2 is generally indicative of a monodisperse sample.
- Surface Charge (Zeta Potential): Determined by Laser Doppler Micro-electrophoresis. This parameter influences colloidal stability and interactions with biological membranes.
- Morphology and Structure: Assessed using Electron Microscopy (SEM, TEM) and Atomic Force Microscopy (AFM).
- Drug Loading and Encapsulation Efficiency: Quantified using techniques like HPLC or UV-Vis spectroscopy after separating free drug from encapsulated drug (e.g., via centrifugation or filtration).
- In Vitro Drug Release Profile: Conducted using dialysis-based methods under sink conditions in physiologically relevant media (e.g., PBS at pH 7.4 and simulated lysosomal fluid at pH 5.0). Sampling at predetermined time points allows for kinetic modeling of release.
Advanced Characterization: Nuclear Magnetic Resonance (NMR) spectroscopy, particularly Diffusion-Ordered Spectroscopy (DOSY), is valuable for determining molecular weight and confirming successful conjugation of drugs or targeting ligands to the polymer backbone [31].
Preclinical Efficacy and Safety Assessment
Preclinical studies must be tailored to the specific PNP mechanism and intended indication.
In Vitro Biological Activity:
- Cell Culture Models: Use relevant cell lines (e.g., MCF-7 for breast cancer) to assess cellular uptake, cytotoxicity (via MTT or Alamar Blue assays), and mechanism of action [98].
- 3D Models: Multicellular tumor spheroids can provide a more physiologically relevant model for evaluating penetration and efficacy [12].
In Vivo Studies:
- Pharmacokinetics/Pharmacodynamics (PK/PD): Evaluate absorption, distribution, metabolism, and excretion (ADME) in rodent models. PNPs often show enhanced area under the curve (AUC) and reduced maximum concentration (Cmax) compared to free drug [99].
- Biodistribution: Use of fluorescent dyes (e.g., DiR) or radiolabels allows tracking of PNP accumulation in target tissues versus off-target organs. The Enhanced Permeability and Retention (EPR) effect is a key rationale for passive tumor targeting [12] [98].
- Toxicology: Repeat-dose toxicity studies in two species (rodent and non-rodent) are required. Specific attention should be paid to potential immunotoxicity, hepatotoxicity, and accumulation in reticuloendothelial system organs (liver, spleen) [100] [102].
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials and Reagents for PNP Development
| Reagent/Material | Function/Application | Examples/Types |
|---|---|---|
| Biodegradable Polymers | Form the nanoparticle matrix; determine biodegradation rate and drug release kinetics. | PLGA, PLA, Chitosan, Polycaprolactone (PCL), Gelatin [98] |
| Functional Polymers | Impart "stealth" properties or enable surface functionalization. | PEG (PEGylation), HPMA (N-(2-Hydroxypropyl)methacrylamide) [12] [98] |
| Targeting Ligands | Enable active targeting to specific cells or tissues (e.g., tumor antigens). | Folic Acid, Peptides (e.g., RGD), Antibodies [12] |
| Characterization Standards | Calibrate instruments and ensure accurate measurement of physicochemical properties. | Latex Nanospheres (for DLS), Zeta Potential Transfer Standard [31] |
| Cell-Based Assay Kits | Evaluate cytotoxicity, cellular uptake, and biological activity in vitro. | MTT/WST-1, LDH, Flow Cytometry Antibody Panels [98] |
CMC and Manufacturing Considerations
Robust chemistry, manufacturing, and controls (CMC) are critical for regulatory approval. Key considerations include:
- Quality by Design (QbD): Implement a systematic approach to development that emphasizes product and process understanding and control. This involves defining a Target Product Profile (TPP) and identifying Critical Quality Attributes (CQAs) [9].
- Scalability and Process Control: Transitioning from lab-scale (e.g., nanoprecipitation) to GMP-compliant manufacturing (e.g., high-pressure homogenization) requires careful process validation and demonstration of product comparability [100] [9].
- Analytical Procedure Validation: All methods used for quality control (e.g., drug assay, related substances, residual solvents, particle size) must be validated according to ICH guidelines (Q2(R1)) to ensure they are suitable for their intended purpose.
- Stability Studies: Conduct long-term and accelerated stability studies to establish a shelf life and recommend storage conditions. These studies should monitor changes in CQAs like particle size, drug content, and impurities over time [100].
The development of PNP-based therapeutics holds immense potential to revolutionize the treatment of myriad diseases, from cancer to resistant infections. Success in this complex field hinges on a deep understanding of the intricate regulatory landscape. By integrating rigorous scientific development—including comprehensive characterization and tailored preclinical studies—with a proactive regulatory strategy that leverages expedited pathways and early agency feedback, developers can significantly enhance their chances of clinical and commercial success. As regulatory science continues to evolve in response to these innovative platforms, a collaborative and transparent approach among researchers, manufacturers, and regulators will be paramount in bringing safe and effective PNP-based therapies to patients in need.
The development of polymeric nanoparticles (PNPs) for drug delivery represents a frontier in modern therapeutics, offering solutions to longstanding challenges such as poor drug solubility, inadequate targeting, and systemic toxicity [12] [75]. PNPs demonstrate remarkable versatility, biocompatibility, and ability to encapsulate diverse therapeutic agents for controlled release [12]. However, the traditional development of PNPs faces significant challenges, as the synthesis of nanomedicines involves numerous parameters, and the complexity of nano-bio interactions in vivo presents further difficulties [103]. The formulation process is influenced by a multitude of critical material attributes (CMAs) and critical process parameters (CPPs) that ultimately determine the critical quality attributes (CQAs) of the final pharmaceutical product [104].
Artificial intelligence (AI) and machine learning (ML) are transforming this landscape by introducing predictive capabilities and data-driven optimization to PNP design [103] [105]. These computational approaches can analyze vast datasets to identify complex patterns that are not apparent through traditional experimentation [105]. The integration of AI is particularly valuable for optimizing nanoparticle transport, tumor penetration, and therapeutic efficacy within multi-scale modeling paradigms [105]. This paradigm shift enables researchers to move beyond resource-intensive trial-and-error methods toward rational design principles guided by predictive modeling [104]. As a result, AI-enhanced PNP design accelerates development timelines while improving the precision and performance of resulting drug delivery systems for applications in cancer therapy, cardiovascular diseases, and central nervous system disorders [12] [106].
AI/ML Applications Across the PNP Development Workflow
Formulation Optimization and Predictive Modeling
Machine learning algorithms excel at navigating complex multivariate relationships inherent in PNP formulation. By integrating with Quality by Design (QbD) frameworks and Design of Experiments (DoE), ML can systematically explore how CMAs and CPPs influence CQAs such as particle size (PS), polydispersity index (PDI), zeta potential (ZP), and encapsulation efficiency (%EE) [104]. This approach was successfully demonstrated in optimizing resveratrol-loaded PNPs, where ML models trained on experimental data could predict nanoparticle characteristics with high accuracy [104]. The ability to predict formulation outcomes without extensive laboratory work represents a significant advancement in pharmaceutical development efficiency.
Different ML algorithms offer distinct advantages for PNP development. Artificial Neural Networks (ANNs) have demonstrated exceptional performance in modeling non-linear relationships in progesterone-loaded solid lipid nanoparticles [104]. Similarly, least-squares boosting (LSBoost) algorithms have accurately predicted the PS and PDI of liposomes loaded with curcumin [104]. These data-driven approaches facilitate a deeper understanding of the relationships between formulation components and their impacts on final product quality, enabling more robust PNP design.
Navigating Biological Interactions and Barriers
Beyond initial formulation, AI plays a crucial role in predicting how PNPs interact with complex biological systems. Multi-scale modeling approaches simulate nanoparticle transport across systemic, tissue, and cellular levels, addressing key processes such as transvascular extravasation, interstitial distribution, and drug release [105]. These computational models can predict biological behavior, including NP-protein interactions, blood circulation time, extravasation into the tumor microenvironment, tumor penetration and distribution, and cellular internalization [103].
The integration of AI with traditional computational models has opened new frontiers in understanding these complex interactions [105]. AI-driven approaches, such as deep learning and reinforcement learning, offer the ability to analyze vast datasets, identify complex patterns, and predict outcomes with remarkable accuracy [105]. This capability is particularly valuable for optimizing PNPs designed to overcome biological barriers such as the blood-brain barrier, mucosal layers, and tumor microenvironments [75]. By predicting these interactions in silico, researchers can design PNPs with improved targeting efficiency and reduced off-target effects.
Toward Personalized Nanomedicine
AI-driven approaches enable the development of patient-specific PNP systems by integrating and analyzing multi-source, high-dimensional data [105]. This capability facilitates precision medicine in cancer therapy, moving beyond one-size-fits-all approaches to account for individual patient characteristics from the outset of treatment design [105]. The potential for personalized medicine is further enhanced by smart PNPs that respond to specific physiological conditions, facilitating targeted and controlled release while minimizing off-target effects [12].
Table 1: AI/ML Applications in PNP Development Workflow
| Development Stage | AI/ML Application | Key Benefits | Representative Algorithms |
|---|---|---|---|
| Formulation Design | Prediction of CMAs and CPPs effects on CQAs | Reduces experimental trials; optimizes particle characteristics | ANN, LSBoost [104] |
| Biological Interaction | Multi-scale modeling of nano-bio interactions | Predicts targeting efficiency; optimizes tissue penetration | Deep Learning, Reinforcement Learning [105] |
| Personalized Design | Integration of patient-specific data | Enables precision medicine approaches; customizes release profiles | Active Learning [105] |
| Manufacturing | Process optimization and quality control | Enhances batch-to-batch consistency; reduces production costs | ML-integrated QbD [104] |
Experimental Protocols for AI-Enhanced PNP Development
Protocol: ML-Integrated QbD for PNP Formulation Optimization
This protocol outlines a systematic approach for developing resveratrol-loaded gelatin type A/tripolyphosphate PNPs using ML-integrated QbD, adapted from established methodologies [104].
Materials and Equipment:
- Polymer: Gelatin type A (Sigma-Aldrich)
- Cross-linker: Tripolyphosphate (TPP)
- Stabilizer: Poloxamer 407 (Sigma-Aldrich)
- Drug: Resveratrol (Sigma-Aldrich)
- Preparation method: Ionic gelation
- Characterization equipment: Dynamic light scattering (DLS) for PS, PDI, and ZP; HPLC for %EE [104]
Procedure:
- Define Quality Target Product Profile (QTPP): Identify target CQAs including PS (100-200 nm), PDI (<0.3), ZP (>|±30| mV), and %EE (>80%) [104].
- Design of Experiments: Implement a full factorial design to investigate the effects of CMAs/CPPs including gelatin concentration, TPP concentration, drug-polymer ratio, and stirring speed [104].
- PNP Preparation:
- Dissolve gelatin type A in distilled water at 40°C
- Add resveratrol to the polymer solution
- Cross-link by adding TPP solution dropwise under stirring at defined speeds
- Maintain stirring for 60 minutes to form PNPs
- Data Collection: Characterize PS, PDI, ZP, and %EE for all experimental runs [104].
- ML Model Development:
- Split data into training and testing sets (typically 80:20)
- Train multiple ML algorithms (ANN, random forest, support vector regression)
- Validate models using cross-validation techniques
- Select optimal model based on prediction accuracy metrics (R², MAE) [104]
- Formulation Optimization: Use the validated ML model to identify the optimal formulation within the design space that meets all CQA targets [104].
- Experimental Verification: Prepare and characterize the optimized formulation to confirm prediction accuracy [104].
Protocol: In Silico Prediction of Tumor Targeting Efficiency
This protocol describes a computational approach for predicting the tumor targeting efficiency of PNPs using multi-scale modeling and AI, based on established computational methodologies [105].
Computational Tools and Models:
- Molecular dynamics software (GROMACS, NAMD)
- Finite element analysis software (COMSOL)
- Machine learning libraries (Scikit-learn, TensorFlow)
- Physiological parameters (tumor vasculature, interstitial pressure, cellular density) [105]
Procedure:
- Data Collection:
- Compile experimental data on PNP properties (size, surface charge, hydrophobicity)
- Collect physiological parameters of target tumor microenvironment
- Aggregate existing in vivo performance data for similar PNPs [105]
- Multi-Scale Model Development:
- Systemic Level: Model blood flow, vascular distribution, and opsonization
- Tissue Level: Simulate transvascular transport (extravasation) and interstitial diffusion
- Cellular Level: Predict cellular uptake, intracellular trafficking, and drug release [105]
- AI Model Integration:
- Train deep learning models on the multi-scale simulation data
- Incorporate stochastic elements to account for biological variability
- Validate models against experimental in vivo data [105]
- Prediction and Optimization:
- Input candidate PNP properties into the validated model
- Predict tumor accumulation and penetration efficiency
- Iteratively refine PNP design to optimize targeting performance [105]
- Experimental Validation:
- Synthesize top-performing PNP designs identified through in silico screening
- Evaluate targeting efficiency in appropriate in vitro and in vivo models
- Compare results with model predictions to further refine accuracy [105]
Table 2: Critical Quality Attributes and Target Ranges for Optimized PNPs
| Critical Quality Attribute (CQA) | Target Range | Analytical Method | Impact on Performance | ||
|---|---|---|---|---|---|
| Particle Size (PS) | 50-200 nm | Dynamic Light Scattering | Affects circulation time, tumor accumulation via EPR effect [12] | ||
| Polydispersity Index (PDI) | <0.3 | Dynamic Light Scattering | Indicates uniformity; affects predictability of behavior [104] | ||
| Zeta Potential (ZP) | > | ±30 | mV | Laser Doppler Anemometry | Influences stability and cellular interactions [104] |
| Encapsulation Efficiency (%EE) | >80% | HPLC/UV Spectroscopy | Determines drug loading capacity and cost-effectiveness [104] | ||
| Drug Release Profile | Sustained release over specified period | In vitro release testing | Affects therapeutic efficacy and dosing frequency [12] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for AI-Guided PNP Development
| Reagent/Material | Function | Examples/Categories | Considerations for AI Integration |
|---|---|---|---|
| Biodegradable Polymers | Structural matrix for PNPs | Gelatin type A, PLGA, Chitosan, PCL [104] | Molecular weight and composition are CMAs for ML models [104] |
| Cross-linking Agents | Stabilize PNP structure | Tripolyphosphate (TPP) [104] | Concentration and addition rate are CPPs in ML optimization [104] |
| Stabilizers/Surfactants | Control particle growth and aggregation | Poloxamer 407, Polysorbates, PEG [12] [104] | Surface modification data used to train targeting models [103] |
| Active Targeting Ligands | Enable specific cell targeting | Antibodies, Peptides, Folates [12] | Ligand density is a key parameter in multi-scale targeting models [105] |
| Stimuli-Responsive Components | Enable triggered drug release | pH-sensitive polymers, thermo-responsive materials [12] | Response thresholds are inputs for controlled release predictions [12] |
Visualizing AI-Driven PNP Development Workflows
AI-Enhanced PNP Design and Optimization Workflow
Multi-Scale Modeling of PNP Biological Journey
The integration of AI and ML into PNP design represents a transformative advancement in nanomedicine development. These technologies enable researchers to navigate the complex multivariate relationships that govern PNP behavior, from initial formulation to biological interactions [103] [104]. The result is an accelerated development timeline and more precisely engineered nanoparticles with optimized therapeutic profiles.
Future developments in this field will likely focus on enhanced personalization, where AI algorithms integrate patient-specific data to design customized PNP systems [105]. Additionally, the growing emphasis on sustainability in nanomedicine production will benefit from AI-driven approaches that optimize manufacturing processes to reduce waste and energy consumption [105]. As these computational methodologies continue to evolve, they will further bridge the gap between in silico predictions and in vivo performance, ultimately advancing precision oncology and accelerating the clinical translation of AI-driven nano-cancer drug delivery systems [105]. The continued refinement of these tools promises to unlock new possibilities in targeted drug delivery, fundamentally enhancing our ability to develop more effective and precise therapeutic interventions for complex diseases.
Conclusion
Polymeric nanoparticles represent a transformative platform in drug delivery, offering unparalleled versatility for controlled release and targeted therapy. The synthesis of knowledge across the four intents confirms that intelligent PNP design—tailoring polymer properties, fabrication methods, and surface functionalization—is paramount to overcoming complex biological barriers and enhancing therapeutic efficacy. While significant challenges in scalability, long-term toxicity, and regulatory approval remain, the future is bright. The convergence of stimuli-responsive polymers, biomimetic strategies, and AI-driven design is paving the way for a new era of precision nanomedicine. Future research must focus on rigorous biocompatibility testing, scalable manufacturing processes, and patient-specific formulations to fully realize the clinical potential of polymeric nanoparticles and usher in a new generation of intelligent therapeutics.
References
- 1. Polymeric Nanoparticles, Nanospheres and Nanocapsules ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3155227/]
- 2. Polymeric Nanoparticles for Biomedical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10821477/]
- 3. in Targeted Polymeric : Unveiling the... Nanoparticles Drug Delivery [https://pubmed.ncbi.nlm.nih.gov/40219222/]
- 4. Engineers develop a way to mass manufacture nanoparticles that... [https://news.mit.edu/2025/engineers-develop-mass-manufacture-nanoparticles-drug-delivery-cancer-tumors-0403]
- 5. Scale-up polymeric-based nanoparticles drug delivery ... [https://www.sciencedirect.com/science/article/pii/S2352952022000111]
- 6. Polymeric Nanoparticles in Targeted Drug Delivery [https://www.mdpi.com/2073-4360/17/7/833]
- 7. Natural and Synthetic Polymers for Biomedical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11055061/]
- 8. Bridging the Gap: The Role of Advanced Formulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579833/]
- 9. Advanced rational design of polymeric nanoparticles for ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925005607]
- 10. Biological Barriers for Drug Delivery and Development of ... [https://www.mdpi.com/1999-4923/16/9/1207]
- 11. Polymeric Nanoparticles for Drug Delivery: Recent Developments and Future Prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7408012/]
- 12. Polymeric Nanoparticles in Targeted Drug Delivery: Unveiling the Impact of Polymer Characterization and Fabrication - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11991310/]
- 13. Cell-Based Drug Delivery Systems - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428288/]
- 14. Factors determining drug delivery system translation [https://www.sciencedirect.com/science/article/abs/pii/S0168365925007795]
- 15. Microfluidic-based nanocarriers for overcoming biological ... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr02322j?page=search]
- 16. Stimuli-Responsive, Cell-Mediated Drug Delivery Systems [https://www.mdpi.com/1999-4923/17/8/1082]
- 17. Current updated review on preparation of polymeric nanoparticles for drug delivery and biomedical applications - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S294982952300013X]
- 18. Factors determining drug delivery system translation [https://pubmed.ncbi.nlm.nih.gov/40865878/]
- 19. Investigation of the protein corona and biodistribution ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961225001577]
- 20. A review on protein corona formation on nanoparticles and ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325009317]
- 21. In vivo Protein Corona Formation: Characterizations ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.646708/full]
- 22. a protein corona-mediated selective targeting system based ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00079c]
- 23. Engineered protein corona sustains stealth functionality of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261846/]
- 24. Investigation of the protein corona and biodistribution profile of ... [https://pubmed.ncbi.nlm.nih.gov/40064138]
- 25. Protein corona formed on lipid nanoparticles compromises ... [https://www.nature.com/articles/s41467-025-63726-2]
- 26. Advanced rational design of polymeric nanoparticles for ... [https://pubmed.ncbi.nlm.nih.gov/40484283/]
- 27. for Polymeric - PMC Nanoparticles Drug Delivery [https://pmc.ncbi.nlm.nih.gov/articles/PMC11086401/]
- 28. Effects of Size and Surface Charge of Polymeric ... [https://www.scirp.org/journal/paperinformation?paperid=65756]
- 29. Effects of particle size and surface charge on cellular ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961210000979]
- 30. Control of Polymeric Nanoparticle Size to Improve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4656075/]
- 31. Characterisation of polymeric for nanoparticles ... drug delivery [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d5nr00071h]
- 32. Polymeric Nanoparticles for Drug Delivery [https://pubmed.ncbi.nlm.nih.gov/PMC11086401]
- 33. Recent Advances in Different Nanoprecipitation Methods ... [https://www.scientificarchives.com/article/recent-advances-in-different-nanoprecipitation-methods-for-efficient-drug-loading-and-controlled-release]
- 34. Nanoprecipitation as a simple and straightforward process ... [https://www.sciencedirect.com/science/article/abs/pii/S0001868621001159]
- 35. Nanoprecipitation process: From encapsulation to drug ... [https://pubmed.ncbi.nlm.nih.gov/28801107/]
- 36. Optimize the parameters for the synthesis by the ionic gelation ... [https://jbioleng.biomedcentral.com/articles/10.1186/s13036-024-00403-w]
- 37. Ionotropic Gelation - an overview [https://www.sciencedirect.com/topics/chemical-engineering/ionotropic-gelation]
- 38. What it is the Ionic Gelation Method? [https://www.ainia.com/en/ainia-news/ionic-gelation-method-a-key-technique-for-the-microencapsulation-of-active-compounds/]
- 39. Formulation development and process parameter optimization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4397346/]
- 40. Critical Review of Techniques for Food Emulsion ... [https://www.mdpi.com/2076-3417/14/3/1069]
- 41. A Comparative Analysis of Nanoparticle Sizing Techniques ... [https://digitalcommons.fiu.edu/undergraduate-journal/vol3/iss1/5/]
- 42. Characterisation of polymeric nanoparticles for drug delivery [https://pubs.rsc.org/en/content/articlelanding/2025/nr/d5nr00071h]
- 43. Measuring particle size distribution of nanoparticle enabled ... [https://www.sciencedirect.com/science/article/pii/S0168365919301130]
- 44. In Vitro Release Study of the Polymeric Drug Nanoparticles [https://pmc.ncbi.nlm.nih.gov/articles/PMC7465254/]
- 45. Polymeric nanoparticles-based targeted delivery of drugs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11845113/]
- 46. Polymeric nanomaterials as a drug delivery system for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417996/]
- 47. Enhancement of EPR Effect for Passive Tumor Targeting [https://www.mdpi.com/2076-3417/15/6/3189]
- 48. Image-guided strategies to improve drug delivery to tumors ... [https://www.sciencedirect.com/science/article/pii/S0006291X25010617]
- 49. Polymer-based nanoparticles for cancer theranostics [https://www.explorationpub.com/Journals/ebmx/Article/101342]
- 50. Recent advances in polymeric nanoparticles for the ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1528752/full]
- 51. Smart Polymeric Nanoparticles for Targeted Delivery and ... [https://www.sciencedirect.com/science/article/pii/S2590183425000341]
- 52. Nanoparticles for Cancer Immunotherapy: Innovations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389689/]
- 53. Present and future of cancer nano-immunotherapy [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02214-5]
- 54. Polymeric Nanoparticles: Production, Characterization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7464532/]
- 55. Nanoparticle technologies in precision oncology and ... [https://www.sciencedirect.com/science/article/pii/S2590156725000386]
- 56. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 57. Nanostructure colloids in ocular drug delivery: advances ... [https://link.springer.com/article/10.1007/s11696-025-04315-x]
- 58. Emerging drug delivery strategies for glaucoma therapy [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00068h]
- 59. Polymeric Nanocarrier-Based Drug Formulations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566902/]
- 60. Polymeric nanoparticles for efficient nose-to-brain delivery [https://pubs.rsc.org/en/content/articlelanding/2025/nr/d5nr00870k]
- 61. Nanotechnology to Overcome Blood–Brain Barrier ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11945272/]
- 62. A formulation dataset of poly(lactide-co-glycolide ... [https://www.nature.com/articles/s41597-025-05520-9]
- 63. Optimization of PLGA Nanoparticle Formulation via ... [https://www.mdpi.com/2072-666X/16/9/972]
- 64. Polymeric Vehicles for Nucleic Acid Delivery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7736472/]
- 65. Landscape of small nucleic acid therapeutics [https://www.nature.com/articles/s41392-024-02112-8]
- 66. Characterization techniques for nanoparticles - RSC Publishing [https://pubs.rsc.org/en/content/articlehtml/2018/nr/c8nr02278j]
- 67. Beyond PEGylation: nanoparticle surface modulation for ... [https://healthnanotechnology.biomedcentral.com/articles/10.1186/s44301-025-00014-4]
- 68. The stealth effect from a medicinal chemist perspective [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360436/]
- 69. PEG alternatives for RNA therapeutics [https://www.nature.com/articles/s41563-025-02408-2]
- 70. Considering the immunogenicity of PEG - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413056/]
- 71. Next-Generation mRNA-LNPs: Strategies to Reduce Anti ... [https://www.biochempeg.com/article/453.html]
- 72. PEGylated PLGA nanoparticles: unlocking advanced ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02410-x]
- 73. the transformative potential of nanotechnology in medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360437/]
- 74. Biocompatible polymeric nanoparticles degrade and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3478073/]
- 75. Advances in nanoparticles in targeted drug delivery–A review [https://www.sciencedirect.com/science/article/pii/S2666845925001163]
- 76. A comprehensive study on the biodegradability ... [https://www.sciencedirect.com/science/article/pii/S2772810224000266]
- 77. Automated and Continuous Production of Polymeric ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2019.00423/full]
- 78. Nanomedicine Scale-up Technologies: Feasibilities and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4245446/]
- 79. Smart nanoparticles for cancer therapy [https://www.nature.com/articles/s41392-023-01642-x]
- 80. Stimuli-Responsive Polymeric Nanosystems for Controlled ... [https://www.mdpi.com/2076-3417/11/20/9541]
- 81. An Overview of Polymeric Nanoparticles-Based Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9893377/]
- 82. Stimuli-Responsive, Cell-Mediated Drug Delivery Systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389507/]
- 83. Advancing endosomal escape of polymeric nanoparticles [https://pubs.rsc.org/en/content/articlehtml/2025/mh/d4mh01781a]
- 84. Green synthesis of polymeric nanoparticles: agricultural ... [https://link.springer.com/article/10.1007/s42452-025-06877-7]
- 85. Using a systematic and quantitative approach to generate ... [https://pubs.rsc.org/en/content/articlelanding/2024/na/d4na00087k]
- 86. Drug Loading in Chitosan-Based Nanoparticles [https://www.mdpi.com/1999-4923/16/8/1043]
- 87. Direct Quantification of Drug Loading Content in Polymeric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7598274/]
- 88. Advances in Doxorubicin Chemotherapy: Emerging Polymeric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293504/]
- 89. The use of nanoparticles for targeted drug delivery in non- ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1154318/full]
- 90. Table 1 List of FDA-approved nanotechnology-based products ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-018-0392-8/tables/1]
- 91. Mind the gap: a survey of how cancer drug carriers are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3889175/]
- 92. Nanotechnologies for Noninvasive Measurement of Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4050079/]
- 93. The Nanocarrier Landscape Evaluating Key Drug Delivery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12232268/]
- 94. Nanoparticles (NPs) Based Drug Delivery System [https://jddtonline.info/index.php/jddt/article/view/7040]
- 95. Nanomaterial-based contrast agents - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10732545/]
- 96. Nanocarrier imaging at single-cell resolution across entire ... [https://www.nature.com/articles/s41587-024-02528-1]
- 97. New Color-Coded Test Quickly Reveals If Medical ... [https://jhtie.jhmi.edu/news/new-color-coded-test-quickly-reveals-if-medical-nanoparticles-deliver-their-payload/]
- 98. Polymeric nanomaterials as a drug delivery system for ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra01788b?page=search]
- 99. Regulatory pathways and guidelines for nanotechnology ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1544393/full]
- 100. FDA Regulatory Pathways for LNP(Lipid Nano Particle) [https://www.regulatorymedicaldevice.com/2025/04/regulatory-pathway-fda-approval-lnp-mrna-therapeutics.html]
- 101. Recent FDA Guidance Addressing Platform Technologies [https://www.wilmerhale.com/en/insights/client-alerts/20240701-recent-fda-guidance-addressing-platform-technologies]
- 102. Bridging the Gap: Regulatory Pathway and Clinical ... [https://link.springer.com/chapter/10.1007/978-981-96-8023-8_12]
- 103. Machine Learning-Enhanced Nanoparticle Design for ... [https://pubmed.ncbi.nlm.nih.gov/40536233/]
- 104. Predictive modeling approach using machine learning ... [https://www.sciencedirect.com/science/article/abs/pii/S0378517325009172]
- 105. Current state-of-the-art in multi-scale modeling in nano-cancer ... [https://cancer-nano.biomedcentral.com/articles/10.1186/s12645-025-00326-1]
- 106. Novel Drug Delivery Systems: An Important Direction for Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11124876/]